When that first step out of bed feels like walking on hot coals, you know it’s time to get serious about your plantar fasciitis. The pain can be overwhelming, but the good news is you can start fighting back right away. The most effective approach for immediate relief is a simple, proven trio: rest, ice, and gentle stretching.
This isn't about a magic cure; it's about calming the fire in your heel and taking back control, starting today.
Your First Steps for Immediate Heel Pain Relief

Waking up to that sharp, stabbing pain is a brutal way to start the day. It’s the classic calling card of plantar fasciitis, an incredibly common condition caused by inflammation of the plantar fascia—that tough band of tissue running from your heel to your toes. If you're dealing with this, you are far from alone.
This isn't some rare, obscure ailment. Plantar fasciitis impacts a huge number of people, affecting around 7% of individuals aged 65 and older worldwide. Here in the United States, it’s a massive issue, driving over one million doctor visits every single year.
So, what can you do when the pain is flaring up? Your first mission is to get that inflammation and tension under control. This is where the time-tested R.I.C.E. method becomes your best friend.
When you're in the throes of acute pain, knowing exactly what to do can feel overwhelming. The table below breaks down the most critical first-response actions to help you manage the pain effectively and start the healing process.
Immediate Actions for Plantar Fasciitis Relief
| Action | Why It Helps | How to Do It |
|---|---|---|
| Rest | This is non-negotiable. It stops the repeated strain that's causing the inflammation in the first place. | Get off your feet. Avoid running, jumping, or long periods of standing. If your job requires it, find every opportunity to sit and unload your feet. |
| Ice | Cold therapy is a powerful, natural anti-inflammatory. It numbs the pain and reduces swelling in the tissue. | Roll a frozen water bottle or can of soda under your arch for 15-20 minutes. The rolling motion also gives a gentle massage. |
| Compression | Applying light pressure helps reduce swelling and can provide a comforting sense of support to the arch. | Use a simple compression sock or an elastic bandage. Make sure it's snug but not tight enough to cut off circulation. |
| Elevation | Gravity is your ally here. Raising your foot above your heart helps fluid drain away from the inflamed area, reducing swelling. | When you're sitting or lying down, prop your foot up on a stack of pillows. |
Think of these actions as your emergency toolkit. By consistently applying them, especially during a flare-up, you can significantly reduce your pain and set the stage for long-term healing.
Gentle Movements to Ease Morning Stiffness
While you need to rest from high-impact activities, staying completely still can actually make things worse by causing the fascia to tighten up. The secret is to introduce gentle, targeted movements that don't put more strain on the tissue.
A simple stretch before you even stand up can make a world of difference.
Pro Tip: While you’re still lying in bed, grab your toes and gently pull them back toward your shin. Hold this for about 30 seconds. Repeat it 3-4 times. This simple move "wakes up" the fascia, making that first step much less jarring.
This isn't about pushing through pain; it's about carefully easing the tension before you ask your foot to bear your full weight.
By combining these strategies, you create a powerful first-response system. After a long day, for example, spend 20 minutes with your foot propped up, rolling it over a frozen water bottle. That one action combines ice, elevation, and a gentle massage. Consistency is everything.
These immediate actions are the first chapter in your recovery story. To build on this foundation, you can learn more about how to help plantar fasciitis in our comprehensive guide. Taking these first steps puts you on the path to finally having pain-free mornings again.
Essential Stretches That Actually Work

Rest is important, no doubt. But if you want to take an active role in your recovery, strategic stretching is your most powerful at-home tool. The right stretches do more than just ease the ache for a little while; they get to the root of the problem by lengthening the tight tissues that are constantly yanking on your plantar fascia.
Think of it like this: your calf muscles and Achilles tendon are often the main culprits in this painful saga. When they’re tight, they put a relentless strain on your heel bone, which in turn pulls on and irritates the plantar fascia. The key is to release that constant tension.
When you're consistent, gentle stretching is one of the most effective ways to manage this condition without invasive procedures. It’s been proven to boost flexibility, get more blood flowing to the area to help it heal, and make you more resilient to future flare-ups.
Target the Source with Calf Stretches
Nine times out of ten, tight calf muscles are the puppet master behind your foot pain. Loosening them up is non-negotiable if you want lasting relief. You actually have two main calf muscles—the big gastrocnemius up top and the smaller soleus muscle underneath it—and you need to stretch both to make a real difference.
The classic wall stretch is perfect for this.
- For the Gastrocnemius (upper calf): Face a wall and place your hands on it for balance. Step one foot back, keeping the leg completely straight with your heel glued to the floor. Now, lean your hips forward until you feel a good stretch high up in your calf.
- For the Soleus (lower calf): Stay in the same position, but now, put a slight bend in the knee of your back leg. Keep that heel down! You should feel this stretch lower down, closer to your Achilles.
Hold each stretch for a solid 30 seconds. You want to feel a pull, but never a sharp pain. Switch legs and repeat 3-4 times on each side. I always tell people to do these at least twice a day, especially after you've been sitting for a while or right before a walk.
Quick tip: Whatever you do, don't bounce. Bouncing can actually cause tiny tears in the muscle, which sets you back. Ease into the stretch and hold it steady. We're aiming to gently lengthen the muscle, not force it.
Direct Relief for Your Plantar Fascia
Stretching your calves takes care of the tension coming from above, but you also need to work directly on the plantar fascia itself. These focused movements can help restore its flexibility and may even help break down some of the minor scar tissue that makes your foot feel so stiff.
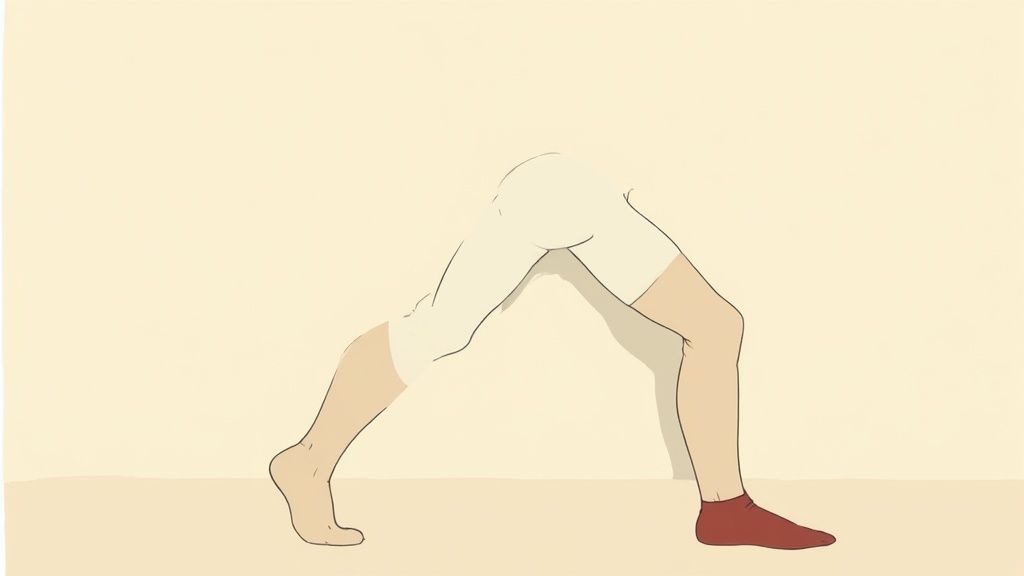
The seated towel stretch is a fantastic one to do before you even put your feet on the floor in the morning.
- Sit on the edge of your bed or a chair with your leg out straight.
- Grab a towel or a resistance band and loop it around the ball of your foot.
- Gently pull the towel toward your body, keeping your knee straight. You’ll feel this deep in the arch of your foot and probably in your calf, too.
Hold it for 30 seconds, relax, and repeat 3-4 times. By doing this before you take those first dreaded steps, you pre-stretch the fascia, warming it up for the day and often dramatically reducing that sharp morning heel pain.
Combine Cold Therapy and Massage
Here’s where you can get really efficient. Why not tackle inflammation and massage the tissue at the same time? Using a frozen water bottle is a classic physical therapy trick for a reason—it works. You get the benefits of a deep tissue massage plus the numbing, anti-inflammatory effects of ice.
It’s incredibly simple to do:
- Freeze a standard water bottle until it’s solid.
- Sit down in a comfortable chair and place the frozen bottle on the floor.
- Roll your sore foot back and forth over the bottle, applying firm but comfortable pressure from your heel to the ball of your foot.
Aim for about 5-10 minutes on each foot. This feels amazing after a long day or after exercise. It soothes the immediate pain, brings down swelling, and helps work out those stubborn knots in the fascia. It's a small habit that can deliver some seriously big results.
Your Shoes: Your Best Friend or Worst Enemy?
Let's talk about what's on your feet right now. The shoes you wear day-in and day-out can either be the key to your recovery or the very reason that stabbing heel pain just won't quit. It’s a hard truth, but that favorite pair of worn-out sneakers or "comfy" flats could be undermining all your efforts.
Making the right footwear choices isn't just a suggestion; it’s a non-negotiable part of any effective treatment plan. Think of your shoes as the first line of defense, giving your inflamed and overworked plantar fascia the structure and stability it's crying out for.
When you wear flimsy, flat, or overly flexible shoes, you're essentially giving your foot permission to overpronate—that's when it rolls too far inward. This motion puts a massive amount of repetitive strain right on the plantar fascia. The right shoes do the opposite. They gently guide your foot into a healthier alignment, taking that stress off the injured tissue with every single step you take.
How to Pick a Supportive Shoe
You don't need a medical degree to spot a good shoe, but you do need to know what to look for. For a moment, forget style and focus entirely on function. A truly supportive shoe has a few non-negotiable features.
Next time you’re shoe shopping, perform these quick tests:
- Check the Heel Counter: This is the back part of the shoe that cups your heel. Give it a good squeeze. Does it collapse like a wet noodle? If so, leave it on the shelf. You need a firm heel counter to keep your heel from wobbling.
- Try the Twist Test: Grab the shoe at the heel and toe and try to wring it out like a dish towel. A good shoe will resist twisting. If it contorts easily, it's not giving you the torsional stability your foot needs.
- Find the Flex Point: A shoe should only bend where your foot bends naturally—right at the ball of the foot. If it folds in half at the arch, it’s a recipe for more pain.
- Look for a Slight Lift: A completely flat shoe can put extra tension on your Achilles tendon, which connects to the plantar fascia. A small heel-to-toe drop of around 10-12mm can offer immediate relief.
And please, avoid walking barefoot on hard surfaces! The same goes for wearing minimalist shoes or flip-flops. It’s like asking an injured ligament to do all the heavy lifting without any support.
Your footwear directly impacts the stress your plantar fascia endures. Choosing a supportive shoe isn't a passive act; it's an active treatment that works for you all day long.
Before we dive into insoles, it's crucial to understand what makes a shoe a friend or foe to your feet. Here’s a quick cheat sheet to help you tell the difference.
Supportive Shoe Features vs Problematic Shoe Features
| Supportive Features (Look for These) | Problematic Features (Avoid These) |
|---|---|
| Sturdy, firm heel counter that doesn't collapse | Flimsy heel that offers no rearfoot control |
| Resists twisting (good torsional stability) | Bends and twists easily in the middle |
| Bends only at the ball of the foot | Folds in half at the arch area |
| A slight heel lift (10-12mm drop) | Completely flat with zero heel-to-toe drop |
| Ample room in the toe box | Narrow or pointed toes that cramp your feet |
| Removable factory insert to add an orthotic | Glued-in insert and a shallow fit |
By prioritizing the features in the first column, you're building a solid foundation for recovery, literally from the ground up.
Adding an Insole: The Secret Weapon
Even the best shoe can get a major upgrade. That’s where a good orthotic insole comes in, providing targeted support right where you need it most. They are a critical tool in this fight.
When you start looking, you’ll find a few different types:
- Cushy Gel Inserts: These feel nice for a minute, but they're all fluff and no substance. They provide cushioning without addressing the root biomechanical problem causing your pain.
- Over-the-Counter Orthotics: This is where you find the real value. A high-quality, podiatrist-designed insole like Samurai Insoles is engineered to correct overpronation. They give you firm, dynamic arch support that realigns your foot and takes the strain off the fascia.
- Custom Orthotics: Molded specifically for your foot by a podiatrist, these are the most expensive option. They're usually best for people with severe or complex foot issues.
For the vast majority of people struggling with plantar fasciitis, a well-designed OTC insole hits the sweet spot of effectiveness and affordability. Samurai Insoles are made to slip right into your supportive shoes, instantly turning them into a therapeutic tool. They control that unstable heel motion and shore up your arch—the two most important factors for healing.
By combining the right shoe with the right insole, you create an environment where your plantar fascia can finally rest and recover. You’re not just masking the pain; you’re helping to fix the problem at its source. To learn more, check out our guide on how to fix plantar fasciitis with a complete recovery plan.
When It’s Time to Call in a Professional

You’ve been doing everything right. You're stretching, icing, and you’ve even invested in better shoes. So what gives when the pain just won't go away?
If you’ve spent weeks diligently following an at-home plan without seeing any real improvement, that’s your cue. It’s not a sign you’ve failed; it's a clear signal that your plantar fasciitis needs a more powerful approach. It's time to bring in a professional.
Trying to just "push through" persistent or severe heel pain is a recipe for chronic problems and a much longer recovery. When that sharp, stabbing pain is still dictating your daily life, a podiatrist or physical therapist can offer the targeted help you need to finally get back on your feet.
What to Expect from Physical Therapy
Visiting a physical therapist (PT) is so much more than just getting a handout with a few stretches. A good PT is like a biomechanical detective for your body, digging into the why behind your pain. They’ll perform a full evaluation, assessing everything from your gait and foot structure to the muscle strength and flexibility all the way up your kinetic chain.
A solid physical therapy program will likely involve:
- Manual Therapy: This is where the therapist gets hands-on, using skilled massage techniques to release the tight fascia, mobilize stiff joints in your foot and ankle, and work out trigger points in your calf muscles. It's a level of relief that’s almost impossible to achieve on your own.
- A Tailored Exercise Plan: Forget generic calf stretches. A PT will prescribe strengthening exercises for the small, intrinsic muscles inside your feet. Building up these tiny muscles gives you better natural arch support, which takes a significant load off your plantar fascia.
- Fixing Your Form: They'll watch you stand and walk to spot issues like overpronation. From there, they'll give you specific cues and exercises to correct your movement patterns, tackling the root cause of the strain.
Exploring More Advanced Medical Treatments
What happens if physical therapy and all your conservative care efforts still aren't enough? At this point, your doctor might bring up more advanced treatments. These are typically reserved for stubborn cases where the inflammation is high and the tissue just isn't healing.
My Two Cents: Think of professional treatments as a necessary tool, not a first resort. They're designed to break that stubborn cycle of chronic pain and inflammation, which then allows all your at-home efforts to finally start working.
One of the most common options is a corticosteroid injection. Your doctor will inject a powerful anti-inflammatory medicine right into the most painful spot on your heel. While it can bring fast, significant relief, the effect is often temporary. It's best used to knock down a severe flare-up, giving you a pain-free window to really commit to your physical therapy exercises.
Another non-invasive option that's become more common is Extracorporeal Shockwave Therapy (ESWT). This treatment uses high-energy sound waves aimed at your heel to stimulate blood flow and jump-start your body’s own healing mechanisms. It’s usually considered when the pain has dragged on for six months or more.
The Game-Changing Role of Night Splints
That searing pain with your first step out of bed happens for a reason: your plantar fascia tightens up overnight while your foot is in a relaxed, pointed position. A night splint is a simple, but often incredibly effective, device that stops this from happening.
It holds your foot in a gentle, dorsiflexed position (think toes pulled slightly toward your shin) all night long. This maintains a light, constant stretch on both your plantar fascia and your Achilles tendon. The result for many people is a dramatic reduction in that dreaded morning pain.
It’s no surprise that the global market for plantar fasciitis treatments, valued at around US$ 778.3 million in 2022, is seeing major growth in these types of devices. Their importance in a complete recovery plan is clear. You can dig deeper into innovations in plantar fasciitis treatment and market trends if you're curious.
Making the decision to see a professional is a proactive step, not a last resort. When you walk into that appointment armed with this knowledge, you can have a much more productive conversation with your doctor and work together to find the best path forward.
Building a Lifestyle That Keeps Flare-Ups Away
Getting rid of that stabbing heel pain is a huge relief. But the real victory? Making sure it stays gone for good. Long-term success isn't just about a few stretches and some ice—it's about weaving new habits into your life that protect your feet from another flare-up.
Think about it: something in your daily routine likely contributed to the problem in the first place. By making a few smart, sustainable changes, you're building a solid defense against re-injury. The idea is to make foot health second nature, not just a temporary fix you do when the pain is bad.
Easing Back Into Your Activities
After weeks of being careful, I know the urge to jump right back into your old routine is powerful. Whether that means running, hitting the gym, or even just taking a long walk, you need a smart plan. Going from zero to sixty is one of the quickest ways to wind up right back where you started: in pain.
A good rule of thumb I always recommend is the 10% rule. Only increase how long or how hard you go by about 10% each week. For instance, if you managed a 20-minute walk without any pain this week, try for a 22-minute walk next week. This slow and steady approach gives your plantar fascia time to adapt and get stronger without getting overwhelmed.
Pay close attention to what your body is telling you. A little muscle soreness after you've been active is okay, but if that sharp, familiar heel pain comes back, that's a major red flag. If it does, just back off for a day or two and try again at an easier pace.
Why Weight Management Matters
It really comes down to basic physics. Every extra pound you carry puts several more pounds of force on your feet with every single step. That constant strain on your plantar fascia makes it much more likely to get inflamed and develop those tiny tears that cause so much grief.
Even losing a small amount of weight can make a massive difference by reducing that load. It’s not a coincidence that studies consistently find a strong link between a higher body mass index (BMI) and the risk of plantar fasciitis. Focusing on a healthy diet and adding low-impact exercises can be a game-changer.
- Swimming and Water Aerobics: You get a fantastic cardio workout without any of the jarring impact on your feet. The water supports you.
- Cycling: Whether you're on a stationary bike or cruising outdoors, cycling is another great way to stay active while being kind to your heels.
- Strength Training: Building more muscle boosts your metabolism, which is a huge help for managing weight in the long run.
Surviving Long Hours on Your Feet
For so many of us—in retail, healthcare, teaching, or manufacturing—standing for eight hours a day isn't optional. If your job has you on your feet all day, especially on hard surfaces like concrete, you have to be proactive.
An anti-fatigue mat is one of the best things you can buy for your workspace. These mats provide a cushioned surface that makes you subconsciously shift your weight, which improves blood flow and eases the constant pressure on your feet.
You should also try to work some "micro-breaks" into your day.
- Do a quick calf stretch against a wall every hour or so.
- When you get a 15-minute break, actually sit down.
- Keep a golf ball under your desk and roll it under your foot to massage the arch.
These little things might not seem like much, but they break the cycle of non-stop strain and really add up. If you're looking for ways to speed up the process, you can find more tips in our guide on how to cure plantar fasciitis in one week.
When you combine these lifestyle tweaks with the right shoes and consistent support from something like Samurai Insoles, you're not just treating the pain—you're building a fortress to keep it from ever coming back.
Got Questions? Let's Get Them Answered
If you're dealing with plantar fasciitis, you've probably got a lot of questions. It's only natural. The internet is filled with conflicting advice, and it can be hard to know what to believe. I've heard them all over the years, so let's cut through the noise and get you some straight, practical answers.
"How Long Is This Going to Take?"
This is always the first question, and for good reason. The honest answer? It really depends on you. For most people who are diligent with their stretches, wear the right shoes, and use good insoles every single day, you can expect to feel a major difference in about 3 to 6 months.
But consistency is everything. I can't stress this enough. If you skip your stretches for a few days or decide to wear those old, flat sneakers "just for a little while," you're going to have setbacks. For those with really stubborn cases that have been lingering for a while, it might take closer to a year to feel 100%. Be patient with your body and stick with the plan.
"Can I Still Work Out?"
Absolutely, but you need to be smart about it. The high-impact stuff that probably contributed to the problem in the first place? That’s off the table for now. You'll need to press pause on activities like running on pavement, jumping rope, or any kind of high-intensity aerobics.
Instead, it's time to shift to exercises that won't punish your heels. Think low-impact.
- Swimming: This is the gold standard. You get a fantastic cardio workout with absolutely zero impact on your feet.
- Cycling: Whether it's a stationary bike or a ride around the neighborhood, cycling keeps the pressure off your plantar fascia.
- The Elliptical: This machine is a great friend to those with heel pain. It gives you a great workout that feels like running, but without the damaging force.
Always, always warm up first and do a gentle stretch for your calves and feet when you're done. If you feel that sharp, stabbing pain while you're exercising, that's your body screaming "stop!" Listen to it.
I tell my patients to think of it as a strategic retreat, not a surrender. You're giving that inflamed tissue the rest it needs to heal, so you can come back stronger. Trying to "push through the pain" is the fastest way to a much, much longer recovery.
"When Should I Actually See a Doctor?"
While you can often manage this at home, there are some clear signs that it's time to bring in a professional. Don't wait around if you notice any of these things. Call a podiatrist or physical therapist right away if:
- The pain is so bad it's changing the way you walk or making it hard to get through your day.
- You've been doing all the right things for a few weeks, and you've felt zero improvement.
- You see any signs of infection like redness, swelling, or the area feels warm to the touch.
- The pain comes with numbness or a tingling feeling. That could mean a nerve issue is involved, which is a different ballgame.
A doctor can give you a proper diagnosis (to make sure it's not a stress fracture or something else) and can open the door to more advanced treatments if your case requires it.
"Are Custom Orthotics Better Than Insoles I Can Buy Online?"
That's a very common myth. People assume that because custom orthotics are expensive and prescribed, they must be better. That’s not always the case.
Honestly, for the vast majority of people suffering from plantar fasciitis, a high-quality, podiatrist-designed over-the-counter insole does the job perfectly. Custom orthotics are really for more complex situations, like severe foot deformities or for people who have tried every other conservative treatment without success.
Starting with a well-designed prefabricated insole is a more affordable, accessible, and often incredibly effective first step.
You're now armed with the right information, and it's time to put it into action. The single most powerful step you can take today is to give your feet the support they're crying out for. Samurai Insoles are specifically engineered to provide that firm, dynamic arch support that takes the strain off your plantar fascia. They effectively turn the shoes you already own into a tool for your recovery.
Start your 60-day no-risk trial and feel the difference at SamuraiInsoles.com



