When that first stabbing pain hits your heel, the biggest question on your mind is always, "How long will this take to go away?" While the typical plantar fasciitis recovery time is anywhere from 3 to 12 months, it's not just a matter of waiting it out. Think of it less as a fixed sentence and more as a journey with distinct stages.
Understanding the Plantar Fasciitis Healing Timeline

Getting over plantar fasciitis isn't like flipping a switch from "pain" to "no pain." It’s more like navigating a set of traffic lights. Each phase has its own rules and goals, signaling how you should approach your daily activities and treatments. Knowing this timeline gives you a clear roadmap, so you can see where you are and what you need to do to get the green light for life as normal.
Your healing journey will generally move through three key stages: acute, subacute, and chronic. The great news is that most people find relief with simple, consistent care. In the first 6 weeks (the acute phase), about 80% of patients notice a big drop in pain just by using conservative treatments like rest and stretching. As you move into the subacute phase (6 weeks to 3 months), that number climbs, with around 90% of people feeling significant relief.
But what if the pain hangs around longer than three months? At that point, the condition is considered chronic, which happens to roughly 20% of people. For a closer look at these timelines and what to expect, you can learn more about how long plantar fasciitis lasts and what influences healing by reading our detailed guide.
To help you track your progress, here’s a quick overview of what to expect in each phase.
Plantar Fasciitis Recovery Phases at a Glance
This table summarizes the typical timeline, symptoms, and primary goals for each stage of plantar fasciitis recovery, helping you identify where you are in the healing process.
| Recovery Phase | Typical Duration | Key Symptoms | Main Goal |
|---|---|---|---|
| Acute Phase (Red Light) | First 6 Weeks | Sharp, stabbing pain, especially with first steps in the morning. High inflammation. | Reduce pain and inflammation. Protect the fascia. |
| Subacute Phase (Yellow Light) | 6 Weeks to 3 Months | Pain lessens to a dull ache. Morning stiffness improves. | Rebuild strength and flexibility. Gradually return to activity. |
| Chronic Phase (Green Light) | 3+ Months | Lingering, sporadic pain, often after activity. Minimal inflammation. | Manage symptoms and prevent re-injury. Full return to activity. |
Understanding these stages is crucial because what helps in one phase might be counterproductive in another. Let's break them down.
The Acute Phase: Red Light
Think of the first few weeks as a "red light" for your foot. This is when the inflammation and pain are at their absolute worst. Your main job here isn't to push through the pain—it's to calm that irritated tissue down.
- Pain Level: Often sharp and most intense with the first steps in the morning or after you've been sitting for a while.
- Main Goal: Reduce inflammation and protect the plantar fascia from any more strain.
- Key Actions: Your best friends during this stage are rest, ice, and gentle stretching. Seriously.
The most common symptom is a sharp, stabbing pain at the bottom of the heel that can travel through the arch. It’s typically most intense with your first few steps after waking up.
The Subacute Phase: Yellow Light
Once that initial, intense pain starts to back off, you’ve entered the "yellow light" phase. This is a time for caution and smart progress. Your plantar fascia is healing, but it's still incredibly vulnerable. One of the most common mistakes people make is jumping back into high-impact activities too soon, which can send you right back to square one.
This phase is all about slowly reintroducing activity while keeping up with your supportive care routines. For a deeper dive into how long this process can take, you can check out our comprehensive guide on how long plantar fasciitis lasts.
Key Factors That Influence Your Healing Speed

Ever wonder why your friend’s heel pain disappeared in a few weeks while you're still limping around months later? The truth is, your plantar fasciitis recovery time is unique to you. There's no universal timeline because several key factors can either hit the accelerator on your healing or slam on the brakes.
Think of it like tending a garden. The final result depends on everything from the soil quality and sunlight to how consistently you remember to water. In the same way, your body's internal environment and daily habits have a huge say in how quickly that torn fascia can mend itself.
Your Personal Health Profile
Your age, weight, and overall health set the stage for recovery. Generally, younger people tend to heal faster because their cellular repair systems are just more efficient. On the flip side, carrying extra weight puts a constant, heavy load on your plantar fascia, which makes it incredibly difficult for the tissue to get the rest it needs to repair.
Certain health conditions can also throw a wrench in the works, especially those that impact circulation or cause chronic inflammation. These factors create your personal starting line for the healing journey.
Foot Structure and Biomechanics
The way your feet are built plays a massive role. If you have naturally flat feet or particularly high arches, you're likely dealing with biomechanical quirks that put extra stress on the plantar fascia. These structural issues are often the root cause of the problem and can be a major roadblock to recovery if you don't address them.
- Flat Feet (Overpronation): When your foot rolls too far inward with each step, it continuously yanks and stretches the plantar fascia.
- High Arches: A very rigid, high arch isn't great at absorbing shock, which means more impact force gets transferred right to your heel and fascia.
- Tight Calf Muscles: If your calves are tight, they pull on your heel bone, creating a constant tug-of-war with your plantar fascia.
Tackling these mechanical issues with the right support is non-negotiable. Using inserts designed for this purpose, like Samurai Insoles, can drastically reduce that daily strain and finally give the tissue a chance to heal.
Key Insight: Your body is a chain of connected parts. A tight calf or a slight flaw in how you walk directly affects your foot, turning a simple step into a source of re-injury.
Your Lifestyle and Commitment to Treatment
This is the one area where you have the most control. Your job, how active you are, and—most critically—your dedication to your treatment plan will make or break your recovery. If you spend all day standing on hard concrete floors without good support, you're actively fighting against your body's attempts to heal.
Plantar fasciitis is incredibly common, affecting an estimated 10% of the population worldwide. The difference between a quick recovery and a long, drawn-out battle often comes down to simple consistency. People who stick to their stretches and wear supportive shoes often feel much better within weeks. But if you ignore the pain or skip your exercises, you can drag the process out for a year or more. You can learn more about how these factors influence what plantar fasciitis feels like and how long it lasts.
Ultimately, ignoring your treatment plan is like trying to heal a cut that you keep picking at. It just won't work.
Proven At-Home Treatments to Speed Up Recovery
When you're dealing with stubborn heel pain, it's easy to feel helpless. But the truth is, you have a lot more control over your healing process than you think. The secret isn't just waiting it out; it's about actively using proven therapies right from your own home. These methods are all about calming down that angry, inflamed tissue while also fixing the underlying problems that got you here in the first place.
This is your practical toolkit for taking charge of your recovery. We'll go over not just what to do, but why each of these strategies is so good at shortening your plantar fasciitis recovery time. Once you understand the "why," building a consistent routine that gets right to the root of the pain becomes so much easier.
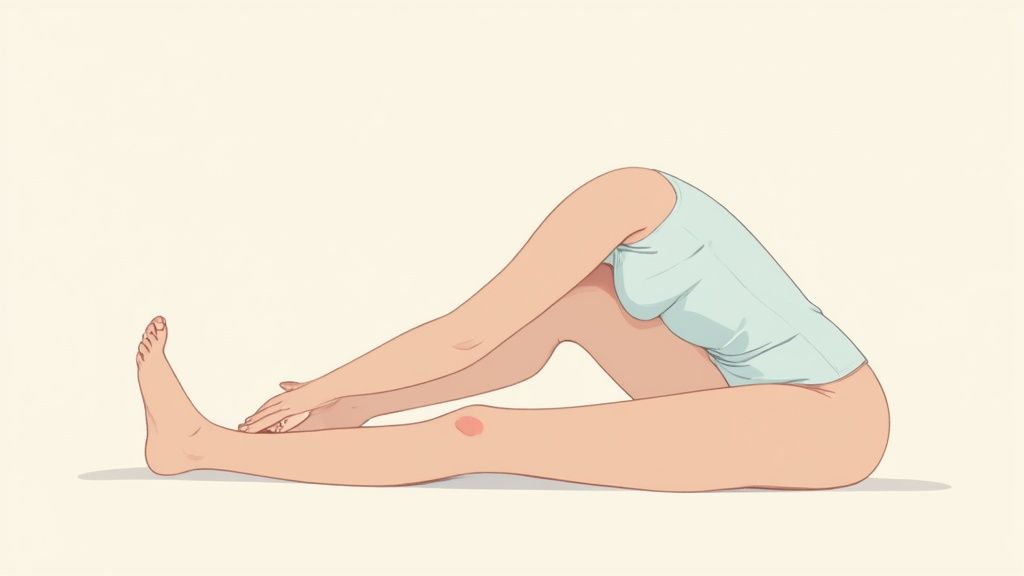
Stretching and Strengthening
Imagine your calf muscles and your plantar fascia are part of the same rope-and-pulley system. If your calves are tight, they're constantly yanking on your heel, keeping that fascia painfully taut. Gentle, consistent stretching is how you release that tension. We're not talking about aggressive, eye-watering pulls, but a gradual lengthening that gives your foot the slack it needs.
At the same time, you need to strengthen the small, intricate muscles inside your foot. Think of them as your body's natural shock absorbers. When these muscles are weak, the plantar fascia has to pick up the slack and ends up overworked and injured.
Here are a few simple exercises to get you started:
- Calf Stretches: A classic for a reason. Lean against a wall with one leg straight behind you, keeping your heel flat on the floor. Hold it for 30 seconds. You're directly targeting those tight muscles that are pulling on your heel.
- Towel Curls: Sit down and place a small towel on the floor under your foot. Using only your toes, scrunch the towel toward you. This is a fantastic way to build up those small, supportive foot muscles.
- Frozen Bottle Rolls: Grab a water bottle, freeze it, and roll your foot over it for 5-10 minutes. This is a great two-for-one: you get a gentle massage and the inflammation-busting power of ice.
For a more comprehensive plan, you can check out a full routine of foot pain relief exercises that build strength and flexibility exactly where you need it.
Using Temperature Therapy and Night Splints
Knowing whether to reach for an ice pack or a heating pad can make a huge difference. In the beginning, when the pain is sharp and inflammation is raging, ice is your best friend. It constricts blood vessels, which helps dial down the swelling and numb the pain. Heat comes in later for that lingering, chronic stiffness, as it boosts blood flow to help heal stubborn tissue.
Key Insight: Ever wonder why that first step in the morning is the absolute worst? It’s because your plantar fascia shortens and tightens up overnight. A night splint is a game-changer here. It holds your foot in a gentle, slightly flexed position while you sleep, preventing that tightening and making your mornings far less dreadful.
The Role of Supportive Footwear and Orthotics
Finally, let's talk about what you put on your feet all day. This is huge. Flimsy shoes, like flat sandals or those old sneakers you love, offer zero support. They let your foot roll inward (overpronate), which puts constant, repetitive strain on the fascia. For recovery, supportive shoes and orthotic inserts aren't just nice to have—they're non-negotiable.
Orthotics work by correcting your foot's alignment and giving your arch the support it's crying out for. This takes the pressure off the plantar fascia, giving it a much-needed break so it can actually heal. This doesn't mean you need to shell out for expensive custom-molded devices, either. A high-quality, over-the-counter insole can often provide all the support you need to get back on your feet, pain-free.
When to Consider Advanced Medical Therapies

So, what happens when you’ve been doing everything right for months? You've been stretching, icing, and resting like a pro, but that stubborn heel pain just won't budge. If conservative treatments haven't made a real dent in your plantar fasciitis recovery time, it might be time to talk to your doctor about stepping things up.
These more advanced options are generally saved for those frustrating, persistent cases where the tissue just seems stuck and needs a serious nudge to get the healing process going again.
Knowing what’s out there helps you have a more informed, confident chat with a specialist about what to do next. The real goal is to get past temporary relief and find a solution that lasts. If you're not sure who to see, learning about what kind of doctor treats plantar fasciitis is the perfect first step to getting the right guidance.
Injections for Pain and Healing
When the pain is severe and just isn’t responding, injections are often the next step. They work in a couple of different ways—some aim to shut down inflammation, while others are designed to kickstart tissue repair right at the source of the problem.
-
Corticosteroid Injections: Think of these as a powerful, targeted anti-inflammatory. They can deliver incredibly fast and significant pain relief, which can feel like a miracle. But they're really a short-term fix. Getting too many can actually weaken the plantar fascia and even risk a rupture, so doctors use them carefully.
-
Platelet-Rich Plasma (PRP) Injections: This is a more modern approach that uses your own body's healing power. A small amount of your blood is taken and spun down to concentrate the platelets. This "healing cocktail" is then injected directly into the damaged fascia to trigger your natural repair systems and encourage long-term tissue rebuilding.
Corticosteroid injections are like calling in the fire department—they put out the raging fire of inflammation right now. PRP therapy, on the other hand, is like hiring a construction crew to come in and rebuild the damaged structure from the ground up for a more permanent fix.
Non-Invasive Regenerative Therapies
If the idea of needles isn't for you, don't worry. There are other advanced technologies that can encourage healing from outside the body. These methods are all about breaking the cycle of chronic pain and degeneration without ever breaking the skin.
One of the most common is Extracorporeal Shockwave Therapy (ESWT). This treatment sends high-energy sound waves directly into your heel. It might sound intense, but think of it as creating tiny, controlled micro-vibrations in the tissue. This process essentially re-awakens the area, telling your body to send a powerful healing response by increasing blood flow and firing up the cells in charge of repair.
It's important to remember that these advanced therapies aren't a first resort. They are usually considered only after you’ve given conservative care a solid try for at least six months without seeing the results you need. They represent a significant step up, offering real hope when the standard playbook just isn’t enough.
Dealing With Plantar Fasciitis When It Just Won't Go Away
For some of us, that nagging heel pain doesn't just stick around for a few weeks. It can drag on for months, turning into what feels like a never-ending battle. If you've been fighting this for six months or more, you’ve officially crossed into what doctors call the chronic phase. This isn't a sign that you've done something wrong; it means the problem inside your foot has changed.
When pain lasts this long, it's often not just about inflammation anymore. The issue has likely shifted from "fasciitis" (inflammation) to "fasciosis" (tissue breakdown). Imagine a rope that's frayed from being pulled too tight for too long, instead of one that's just temporarily irritated. The tissue itself is starting to weaken, which explains why the old "rest and ice" strategy just isn't cutting it anymore.
So, Why Does It Become a Long-Term Problem?
Certain things can stack the deck against a quick recovery. It’s not about a single misstep, but more of a perfect storm of factors that keep the fascia from ever getting the chance to heal completely.
Here’s what often keeps the pain cycle going:
- Constant Strain: If your job requires standing on concrete all day or you keep up with high-impact sports without the right support, the tissue never gets a break.
- Ignoring Your Foot's Structure: Underlying issues like flat feet or really tight calf muscles are a huge factor. If they aren't addressed, they keep pulling on the fascia, guaranteeing it stays stressed.
- On-Again, Off-Again Treatment: Being diligent with stretches and wearing your orthotics for a week, then forgetting for two, creates a frustrating cycle of almost getting better, only to slide right back into pain.
The journey with chronic plantar fasciitis can be a grind, no doubt. But it's so important to keep things in perspective. Even though it feels like forever, long-term studies show that most people do get better.
Expert Insight: Chronic plantar fasciitis isn't a life sentence. It’s your body sending a clear signal: you need a smarter, more consistent game plan that gets to the root cause of the tissue damage, not just the pain itself.
A Realistic Timeline for Long-Haul Recovery
Even when recovery feels impossibly slow, the numbers are actually on your side. Research has shown that plantar fasciitis can be a stubborn beast, with symptoms sometimes lasting for years. One study followed up with patients and found that 29% still had some pain after an average of 5.2 years. This highlights that for some people, it can become an issue that flares up from time to time. The study also pointed out that women and people with pain in both feet were more likely to face these long-term challenges. You can read more about these findings on plantar fasciitis chronicity.
That might sound a little bleak at first, but flip it around: it means over 70% of the people in that same group eventually found lasting relief. The real lesson here is that while the road might be long, sticking with a well-rounded approach is what gets you to the finish line.
It becomes less about a quick fix and more about consistent management—things like wearing supportive insoles such as Samurai Insoles every single day, committing to your strengthening exercises, and learning to adjust your activities when you feel a flare-up coming on.
Common Questions About Your Recovery
It's completely normal to have questions as you work your way through recovery. In fact, it's a good sign—it means you're paying attention to what your body is telling you. Getting clear, straightforward answers can make all the difference, so let's tackle some of the most common things people wonder about as they heal from plantar fasciitis.
Knowing what to expect can help you navigate the ups and downs with a lot more confidence.
Can I Still Exercise with Plantar Fasciitis?
Yes, and you absolutely should! The trick is to be smart about how you exercise. For now, you need to put high-impact activities on hold. Anything that involves pounding your heel—like running, jumping, or high-impact aerobics—is going to aggravate the healing tissue.
Instead, it's time to get friendly with low-impact workouts. You have plenty of great options:
- Swimming and Water Aerobics: Water is your best friend right now. It supports your body weight, taking almost all the pressure off your feet while still giving you a fantastic workout.
- Cycling: Hopping on a stationary bike or heading out for a ride is a great choice. Cycling puts the pressure on the balls of your feet, mostly sparing your sensitive heel.
- Elliptical Machines: These machines are brilliant because they mimic the motion of running without the jarring impact. You get the cardio without the pain.
The most important rule? Listen to your body. If you feel that sharp, familiar pain in your heel, that’s your signal to stop. And don't forget to gently stretch before and after every session—it's non-negotiable for keeping things flexible.
How Do I Know if My Plantar Fasciitis Is Improving?
Staying motivated is so much easier when you can see you're making progress. The biggest and most welcome sign is a change in your morning routine. That awful, stabbing pain with your first few steps out of bed will start to fade. The "morning hobble" will become less and less intense.
You'll also notice other positive changes, like being able to stand for longer without your heel starting to ache or feeling less tenderness when you press on the sore spot.
A Practical Tip: To track your progress objectively, rate your pain on a scale of 1 to 10 each morning. Just jot it down in a notebook or a note on your phone. As long as the numbers are generally trending down over several weeks, you know you're on the right track.
Why Does My Heel Hurt Most in the Morning?
This is the classic, tell-tale symptom of plantar fasciitis. It all comes down to what happens while you sleep. Your foot naturally relaxes into a pointed-toe position, which allows the plantar fascia ligament to shorten and tighten up for hours on end.
Then, when you swing your legs out of bed and put weight on your foot, you’re suddenly stretching that cold, contracted tissue. Think of it like trying to quickly stretch a cold rubber band—it's stiff and can even cause tiny tears, which is what creates that sharp pain. This is exactly why night splints work so well; they keep your foot in a gentle, flexed position all night, preventing the ligament from tightening up in the first place.
Is It Normal for Recovery to Have Good and Bad Days?
Absolutely. Healing is almost never a straight line. It's much more of a "two steps forward, one step back" kind of journey. Experiencing good days where you feel great, followed by a flare-up, is a totally normal part of the process.
Usually, you can trace a "bad day" back to a specific trigger. Maybe you were on your feet too long, wore the wrong shoes, or pushed a little too hard during an activity. Don't let these moments discourage you. Instead, look at them as learning opportunities. They teach you about your body's limits and help you identify your personal triggers. As long as the overall trend is toward less pain, you're still winning.
Navigating the ups and downs of recovery is a whole lot easier when your feet get consistent, reliable support. Samurai Insoles are designed to give your feet the stability and cushioning they need to heal, taking the daily strain off the fascia and helping you avoid those painful setbacks. Give your feet the support they deserve. Explore Samurai Insoles today.



