If you’ve ever had to brace yourself before taking that first step out of bed, you know the tell-tale sign of plantar fasciitis. That sharp, stabbing pain in your heel isn't just a random ache—it's your body sending a clear signal that something is wrong. The good news is, you can fix it. It just takes a smart approach that combines rest, the right kind of stretches, and supportive footwear or insoles to take the load off that angry ligament.
Why Does That First Step in the Morning Hurt So Much?
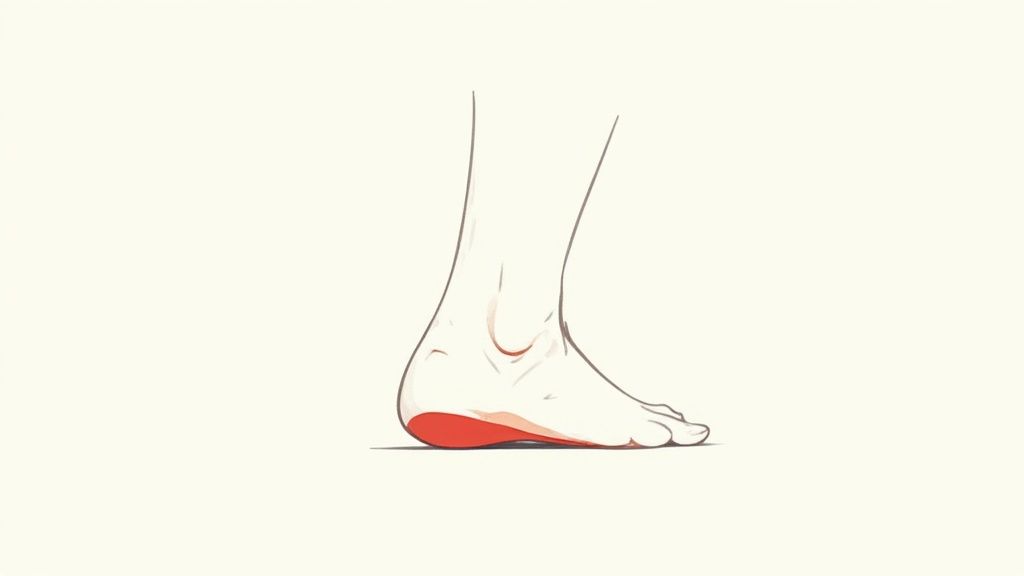
That searing pain that shoots from your heel can bring your morning to a screeching halt. It's a truly awful feeling, but there's a simple mechanical reason behind it. The source of the pain is your plantar fascia, a thick, powerful ligament that runs along the sole of your foot. Think of it as a bowstring connecting your heel to your toes, holding up your arch with every step you take.
Understanding the Strain on Your Foot
While you're asleep, your foot is relaxed, and that hard-working ligament gets a chance to shorten and tighten up. The problem comes when you swing your legs out of bed and put your full weight on it. That first step suddenly yanks on the contracted, inflamed tissue, causing tiny tears and that signature sharp pain. It's like pulling hard on a frayed rope that's gone stiff overnight.
After a few minutes of hobbling around, the fascia starts to warm up and stretch out, which is why the pain usually eases into a dull throb. But don't be fooled—the underlying strain is still there, just waiting to flare up again after you've been sitting at your desk or driving for a while.
The pain you feel isn't just a nuisance; it's a direct signal that your plantar fascia is overloaded and desperately needs relief. Pushing through it often leads to chronic pain and a much tougher road to recovery.
This isn't some rare, obscure problem. Far from it. Plantar fasciitis is incredibly common, affecting about 10% of the global population at some point in their lives. Here in the United States, around 2 million people see a doctor for it every single year. It’s one of the leading causes of heel pain, especially for adults between 40 and 60. If you're interested in the data, you can explore the prevalence of plantar fasciitis statistics for a deeper dive.
What’s Causing the Pain in the First Place?
Plantar fasciitis rarely happens because of one specific injury. Instead, it’s almost always the result of repetitive stress that builds up over time, eventually overloading the ligament. Figuring out what's contributing to your pain is the key to finding lasting relief.
To help pinpoint the cause, let's look at the most common culprits. This table outlines the factors that often lead to plantar fasciitis.
Common Risk Factors for Plantar Fasciitis
| Risk Factor Category | Specific Examples |
|---|---|
| Lifestyle & Occupation | Standing or walking for long hours on hard surfaces (e.g., nurses, teachers, retail workers). |
| Physical Activity | Suddenly increasing the intensity of high-impact exercises like running, dancing, or jumping. |
| Footwear Choices | Frequently wearing shoes with poor arch support, like flat sandals, flip-flops, or old, worn-out sneakers. |
| Biomechanical Issues | Having flat feet (overpronation) or unusually high arches, which can affect how weight is distributed. |
| Body Weight | Excess weight places significantly more stress on the plantar fascia with every step. |
| Age & Tight Muscles | As we age, the fat pad on the heel can thin out. Tight calf muscles or Achilles tendons also pull on the heel bone. |
Recognizing which of these factors apply to you is your first real step toward getting better. By addressing the root cause—whether it’s your shoes, your workout routine, or your daily habits—you can start to heal the tissue instead of just managing the pain.
Practical Home Remedies for Immediate Pain Relief

When a plantar fasciitis flare-up hits, that stabbing heel pain can bring your day to a screeching halt. What you need are simple, effective ways to calm things down and get comfortable right now. This is where a few go-to home remedies become your first line of defense. Think of it as first aid for your foot—quick actions that provide immediate relief while you work on the bigger picture of healing.
The most tried-and-true method for that acute, throbbing pain is the R.I.C.E. method: Rest, Ice, Compression, and Elevation. It might sound basic, but each step is crucial for getting pain and swelling under control.
The R.I.C.E. Method for Foot Pain
-
Rest: This one is non-negotiable. You have to stop doing whatever is making the pain worse, especially high-impact activities like running or jumping. Giving that inflamed ligament a real break is the first step toward recovery.
-
Ice: Cold therapy is a fantastic way to dial down inflammation and numb that sharp pain. Try icing for 15-20 minutes at a time, a few times throughout the day.
-
Compression: Wrapping your foot with an elastic bandage or pulling on a compression sock can really help manage swelling. That gentle, supportive pressure on the arch can also take the edge off the throbbing.
-
Elevation: Whenever you’re sitting down, prop your foot up. Getting it above the level of your heart helps gravity do its job, pulling excess fluid away from the inflamed tissue.
My Favorite Tip: Grab a standard water bottle, freeze it, and then gently roll your foot over it for about 15 minutes. It’s the perfect two-for-one: you get the numbing power of an ice pack combined with a gentle massage that stretches out the entire plantar fascia.
Over-the-Counter Pain Relief
Sometimes, rest and ice just aren't enough to cut through the pain. That's when over-the-counter (OTC) pain relievers can be a really helpful, but temporary, tool.
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) or naproxen (Aleve) are usually the first recommendation. They’re effective because they tackle both the pain signals and the underlying inflammation causing them. Acetaminophen (Tylenol) can also help with the pain itself but doesn't have that same anti-inflammatory punch. You can explore a variety of pain relievers to find what works best to take the edge off your discomfort.
It’s important to see these medications as a short-term bridge, not a permanent fix. They're there to manage the worst of the symptoms so you can comfortably do the stretches and other therapies that lead to long-term healing. As the pain subsides, you might find our guide on how to help plantar fasciitis helpful for what to do next.
Just remember to always use OTC medications as directed on the label and talk to your doctor if you find yourself needing them for more than a week or so.
Targeted Stretches Can Make All the Difference

While ice packs and rest can give you some temporary relief, targeted stretching is where the real, long-term healing begins. The problem with plantar fasciitis often isn't just in your foot. It's usually connected to tightness in other areas, especially your calves. Gentle, consistent stretching is really the best way to lengthen those tissues, take the pressure off your heel, and get your flexibility back.
But you have to do the right stretches, the right way.
For instance, one of the most powerful things you can do is stretch before your feet even hit the floor in the morning. Why does that first step out of bed hurt so much? Because your fascia tightens up overnight. A quick, gentle stretch before you stand up can prepare it for the day and make a world of difference.
The Stretches I Recommend to All My Clients
The goal here is simple. We need to stretch the plantar fascia ligament itself and also loosen up the calf muscles and Achilles tendon, since they're constantly pulling on your heel bone. If you can work these into your daily routine, you're building a strong foundation for recovery.
1. The Classic Wall Calf Stretch
This one is a classic for a reason. It targets the big muscle in your calf (the gastrocnemius) and does a fantastic job of reducing that constant pull on your heel.
- Find a wall and stand about an arm's length away.
- Put your hands on the wall for balance. Step one foot back, keeping that leg completely straight with your heel firmly on the floor.
- Now, bend your front knee. You should feel a nice, gentle stretch running up the calf of your back leg.
- Hold it there for 30 seconds. You want to feel a good pull, but never pain.
- Switch to the other leg and do this 3-4 times on each side.
2. The Seated Towel Stretch
This is my go-to for directly targeting the plantar fascia. It gives you a focused stretch right where you feel that nagging pain.
- Sit down on the floor, legs straight out.
- Grab a towel (a yoga strap or even a belt works too) and loop it around the ball of your sore foot.
- Keeping your knee straight, gently pull the towel toward your body. You'll feel the stretch along the arch and bottom of your foot.
- Hold this for a solid 30 seconds and repeat 3-4 times.
I can't stress this enough: don't overdo it. So many people think a harder stretch is a better stretch, but with plantar fasciitis, that's a huge mistake. Aggressively yanking on the fascia can just make the inflammation worse and set you back. Listen to your body—if you feel a sharp pain, ease up.
Don't Forget to Strengthen Your Feet
Stretching is for flexibility, but strengthening is for support. If the small, intrinsic muscles in your feet are weak, they can't properly support your arch, which puts even more strain on the plantar fascia. These simple exercises might feel a little silly, but they work.
Marble Pick-Ups
Think of this as physical therapy disguised as a game. It's incredibly effective for building up those tiny foot muscles.
- Sit in a chair, feet flat on the floor.
- Scatter 15-20 marbles on the floor next to an empty bowl.
- Using just the toes of your affected foot, pick up one marble at a time and drop it into the bowl.
- Keep going until the floor is clear.
Towel Curls
No marbles? No problem. A small hand towel works just as well for this one.
- Stay seated in your chair and lay a small towel flat on the floor in front of you.
- Keep your heel planted on the ground and use only your toes to scrunch the towel, pulling it toward you.
- Once it’s all bunched up, push it back out flat.
- Repeat the whole cycle 10-15 times.
The real secret to making these stretches and exercises work is consistency. Doing them every single day—especially first thing in the morning and after you've been sitting for a while—is the most important part of tackling plantar fasciitis. It's that steady effort that slowly but surely retrains your muscles and ligaments, paving the way for relief that actually lasts.
How to Choose a Shoe That Soothes Your Feet
Your shoes can be your worst enemy or your best friend when you're fighting heel pain. Think about those flimsy, worn-out sneakers or flat sandals in your closet. With every step, they force your plantar fascia to stretch and strain, making the problem worse.
Switching to truly supportive footwear is non-negotiable for recovery. A good shoe acts like an external support system, taking the pressure off that inflamed ligament. It gives your foot a chance to heal, even when you're on the go. When you shop, you're not just looking for something that feels soft; you need specific features that counter the stress causing your pain in the first place.
The Anatomy of a Supportive Shoe
Finding the right shoe isn’t as complicated as it might seem. You just have to know what to look for. For a moment, forget about the brand name and focus on the structure of the shoe itself.
-
Firm Arch Support: This is the big one. A supportive shoe must have a defined, sturdy arch that mirrors your own. This prevents your foot from rolling inward (a common issue called overpronation) and takes a massive amount of strain off the plantar fascia.
-
A Deep, Cushioned Heel Cup: Look for a shoe that cradles your heel. This feature is crucial for absorbing the shock that travels up your leg with every footstrike. It provides a stable foundation and protects your already-sore heel.
-
A Rigid Sole: Here’s a simple test you can do in any shoe store. Hold the shoe by the heel and toe and try to bend it in half. If it folds easily in the middle, it’s a no-go. A properly supportive shoe should only bend where your foot naturally does—at the ball of the foot.
Your best bets are often running shoes (even just for walking), supportive clogs, or casual shoes built with orthotic support in mind. The shoes to avoid at all costs? Thin flip-flops, ballet flats with zero structure, and any old sneakers that have lost their shape and support.
From Good Shoes to Great Shoes with the Right Insoles
Even the best shoe off the shelf might need a little boost to give you the targeted relief you need. This is where orthotic insoles become your secret weapon, turning a decent shoe into a personalized pain-relief machine. You generally have two options here.
Over-the-Counter (OTC) Insoles: These are easy to find and can offer fantastic arch support and cushioning. High-quality options like Samurai Insoles are often designed by podiatrists to specifically address problems like overpronation, a major trigger for plantar fasciitis. They strike a great balance between cost and effectiveness.
Custom Orthotics: If OTC insoles aren't cutting it, a podiatrist can prescribe custom orthotics. These are molded to the exact shape of your feet, offering the highest level of correction for severe biomechanical issues.
To make it easier to spot the good from the bad when you're shopping, here’s a quick comparison of what to look for and what to run away from.
Supportive Shoe Features vs. Problematic Shoe Features
| Helpful Feature | Why It Works | Problematic Feature | Why It's Harmful |
|---|---|---|---|
| Firm Heel Counter | Stabilizes the heel and prevents it from rolling, reducing stress on the plantar fascia. | Flimsy Heel | Allows for excessive foot motion, increasing strain with every step. |
| Rigid Midsole | Provides consistent arch support and prevents the shoe from collapsing under pressure. | Flexible Middle | Offers no support to the arch, forcing the plantar fascia to work harder. |
| Deep Heel Cup | Cradles the heel's fat pad, maximizing natural cushioning and shock absorption. | Flat Footbed | Provides no stability or shock absorption, leading to direct impact on the heel. |
| Slight Heel Lift | A small drop from heel to toe (around 10-12mm) can reduce strain on the Achilles and fascia. | Zero-Drop or Negative Heel | Can increase the stretch and load on the plantar fascia, worsening pain. |
Choosing the right footwear is a game-changer. It creates a stable, supportive foundation that finally gives your feet the environment they need to heal. This is especially true for those with unique foot structures, like flat feet. If that sounds like you, learning how to choose the best shoes for athletes with flat feet can provide even more tailored guidance.
When Your Heel Pain Warrants a Doctor's Visit
While you can often tackle heel pain at home, sometimes self-care just isn't enough. If that stubborn pain is seriously disrupting your daily life, that’s your cue to get a professional opinion. Knowing when to make that call is key to stopping a nagging issue from turning into a chronic problem.
Have you been diligently stretching, icing, and resting for a few weeks with little to no improvement? It's time to book an appointment. You should also see a doctor if the pain is so severe it’s getting in the way of normal activities, like walking through the grocery store or doing your job. That’s a sign that you need a higher level of care.
What to Expect at Your Appointment
A doctor’s visit for heel pain is usually pretty straightforward. It’ll start with a simple conversation and a physical exam. Your doctor will want to know about your symptoms, your activity levels, and what seems to make the pain better or worse.
Then, they’ll gently press on your foot and heel to find the exact spot that’s tender. This is a classic way to confirm plantar fasciitis.
Sometimes, your doctor might want a clearer picture of what’s happening inside your foot. An X-ray can help rule out other problems, like a stress fracture or a heel spur. An ultrasound is another tool they might use to get a detailed look at the plantar fascia itself, which can reveal any thickening or damage to the ligament.
A trip to the doctor isn't about starting from square one. It's about confirming the diagnosis and escalating your care when home remedies have hit a wall.
Advanced Treatment Options
If your pain isn't getting better with at-home efforts, seeking professional consultations can provide a clear diagnosis and a more powerful treatment plan. This unlocks a whole new level of options you can't access on your own.
Here are some of the things a doctor might recommend:
- Formal Physical Therapy: A physical therapist can guide you through specific stretches and strengthening exercises designed just for you. They can also use hands-on techniques to improve your foot's mobility.
- Corticosteroid Injections: For really intense inflammation, an injection can deliver powerful anti-inflammatory medicine right to the source of the pain, often bringing significant short-term relief.
- Extracorporeal Shockwave Therapy (ESWT): This non-invasive treatment uses sound waves to kickstart the healing process in the damaged ligament.
- Night Splints: Your doctor may suggest wearing a splint while you sleep. This device holds your foot in a gently flexed position, which stops the plantar fascia from tightening up overnight.
Treatments for plantar fasciitis are always improving, partly because we have a better understanding of the condition and how it affects people. This has led to new, approved therapies and a growing market for solutions. If you’re curious about how long recovery might take, our guide on how long plantar fasciitis can last provides some great context for your conversation with your doctor.
Answering Your Top Questions About Heel Pain
Once you start dealing with plantar fasciitis, a lot of questions come up. It's totally normal to feel a bit lost in the sea of advice out there. I've been there, and I've helped countless others navigate it. Let's tackle some of the most common questions I hear so you can get some clarity and get back on your feet.
How Long Does Plantar Fasciitis Take to Heal?
This is the big one, isn't it? The honest answer is, it depends. For most people who stick to a solid routine—stretching, icing, and wearing the right footwear—the pain usually gets much better within three to six months. In some stubborn cases, though, it can hang around for up to a year.
The real game-changer here is consistency. Healing isn't about finding a single magic bullet; it’s about the small things you do every single day. If you commit to your stretches and stop wearing flimsy, unsupportive shoes, you'll be on the fast track to recovery. Trying to "power through" the pain will only make it last longer.
If you want to dive deeper into the recovery timeline, we have a whole article on what to expect as you heal from plantar fasciitis.
Is It Okay to Walk or Run with Plantar Fasciitis?
Exercising when your heel is screaming at you is a real tightrope walk. During a bad flare-up, you absolutely want to avoid high-impact activities like running on asphalt or doing jumping exercises. That kind of pounding will just aggravate the ligament and set your healing back.
But that doesn't mean you should just sit on the couch. In fact, gentle, low-impact movement can be beneficial by keeping blood flowing to the area.
Here are a few smart swaps to consider:
- Instead of pounding the pavement, try swimming or hopping on a stationary bike. You get a great workout without the jarring impact.
- If you love walking, stick to softer surfaces like a running track or a grassy park. And make sure you're wearing very supportive shoes with good insoles.
- Pay attention to what your body is telling you. If any activity makes your heel pain spike, that’s your cue to stop. You're pushing it too hard, too soon.
Your pain is your best guide. A great rule of thumb is to keep any discomfort below a 4 on a 1-to-10 pain scale. If it creeps higher, it’s time to back off.
Will Plantar Fasciitis Come Back After It Heals?
Unfortunately, yes, it can. Plantar fasciitis often returns if you don't address the root cause of the problem. If you get rid of the pain and then immediately go back to wearing unsupportive shoes and skipping your calf stretches, you're rolling out the welcome mat for its return.
To keep it from coming back, you need to make the good habits you learned during recovery a permanent part of your life. Think of supportive insoles and daily stretching not just as a temporary fix, but as essential long-term maintenance for your feet. This is especially critical if you have underlying issues like flat feet or high arches.
Are Night Splints Actually Helpful?
Night splints can be a real game-changer, especially for that awful, sharp pain with your first few steps in the morning.
So how do they work? They hold your foot in a gentle dorsiflexion (flexed) position while you sleep. This prevents your plantar fascia ligament and calf muscles from tightening up overnight.
By keeping everything lightly stretched, you avoid that agonizing shock when you first step out of bed. They might feel a little strange to wear at first, but many people find that using a night splint consistently makes a huge difference in their morning pain levels and helps the healing process along.
Finding your way out of heel pain really comes down to giving your feet the right kind of support. Samurai Insoles were specifically designed by a podiatrist to combat overpronation, which is one of the biggest culprits behind plantar fasciitis.
Give your feet the relief they deserve. Take a step toward a pain-free life and explore our podiatrist-designed insoles.



