That sharp, throbbing ache in your heel after a long day on your feet? It’s not just simple fatigue. It’s your body sending a clear signal that something is wrong.
Why Your Heels Hurt After a Long Day
Our feet are marvels of engineering, but they aren't invincible. When you stand for hours, especially on hard surfaces like concrete or tile, you’re putting a huge amount of continuous pressure on a very small area. This is why heel pain after standing all day is such a common gripe for people in professions like nursing, retail, teaching, and manufacturing.
The main culprit behind this pain is a thick, tough ligament that runs along the bottom of your foot called the plantar fascia. Picture it as your foot's natural shock absorber, connecting your heel to your toes and supporting the arch. When you walk, it flexes and spreads the load. But when you stand still, the pressure just sits there.
The Problem with Standing Still
It might sound easy, but just standing in one spot is incredibly demanding on your body. When you walk, your leg muscles contract and relax, which helps pump blood back to your heart. Standing still robs you of this natural pump.
This forces your muscles to stay tensed up without a break, leading to a few problems:
- Constant Strain: The plantar fascia gets pulled taut like an overstretched rubber band, putting it under constant tension.
- Tiny Tears: This relentless strain can cause tiny, microscopic tears in the ligament, which is what leads to inflammation and that sharp, stabbing pain.
- Poor Circulation: Staying in one position can slow down blood flow, which means less oxygen and nutrients get to your tired muscles, and healing slows to a crawl.
The science backs this up. Studies have shown that standing for more than four hours a day can double the complaints of low back pain, and heel pain often comes along for the ride. In fact, about one in seven workers feels physically burdened by having to stand for most of their shift. You can read more about the effects of prolonged standing and the musculoskeletal issues it can cause.
This combination of strain, inflammation, and poor circulation is why the pain feels so intense—it’s a physical response to being overworked. It's not just in your head; it’s a genuine injury happening on a small scale, and it can easily lead to chronic conditions like plantar fasciitis if ignored.
To help you figure out what’s going on, here’s a quick breakdown of common symptoms and what you can do about them right now.
A Quick Look at Your Heel Pain
| Symptom | Likely Cause | Quick Relief Action |
|---|---|---|
| Sharp, stabbing pain in the heel, especially in the morning. | Plantar Fasciitis | Gently stretch your foot before getting out of bed. Roll a frozen water bottle under your arch. |
| A deep, bruise-like ache in the center of the heel. | Heel Pad Bruise | Ice the area for 15-20 minutes. Avoid walking barefoot on hard surfaces. |
| Swelling and tenderness at the back of the heel. | Achilles Tendinitis | Rest and ice. Perform gentle calf stretches. Avoid activities that strain the Achilles. |
| Pain that worsens after, not during, activity. | General Overuse/Strain | Elevate your feet. Wear supportive shoes even around the house. Consider compression socks. |
Remember, these are just quick fixes. If your pain is severe or doesn't improve, it's always best to see a healthcare professional for a proper diagnosis.
Plantar Fasciitis: The Main Culprit Explained

If your heel pain after standing all day comes with a nasty, stabbing sensation when you first get out of bed, you're almost certainly dealing with plantar fasciitis. It's the single most common reason for heel pain, especially for folks who spend their workdays on their feet.
Picture the plantar fascia. It's a thick, tough band of tissue, kind of like a bowstring, that stretches from your heel to your toes along the bottom of your foot. Its whole job is to support your arch and act as a shock absorber. It’s designed to handle a lot, but everyone has a breaking point.
How Standing Turns Up the Pain
When you're on your feet for hours at a time, especially on hard floors like concrete, you're putting that ligament under constant, relentless tension. Imagine stretching a rubber band as far as it can go and just holding it there for an entire workday. That immense strain can eventually lead to tiny micro-tears in the tissue.
Your body’s natural reaction is to send in the inflammation crew, and that’s what causes the pain. This also explains the infamous morning hobble. As you sleep or sit, the ligament gets a chance to tighten up. Then, when you take those first few steps, you're suddenly yanking on that sore, shortened tissue. Ouch.
This is way more than just a little foot ache; for many, it can be truly debilitating. The impact is especially hard on people whose jobs demand they stay standing.
A study on sales promotion workers, for instance, found that a staggering 30.3% had plantar fasciitis. The condition was directly tied to more intense pain and limitations that tanked their quality of work.
Seeing this connection is the first real step toward relief. The pain isn't just happening to you; it's a direct result of the mechanical stress your feet are under.
Recognizing the Telltale Signs
So, how can you know for sure if plantar fasciitis is what's going on? A proper diagnosis from a professional is always the best move, but the symptoms are usually pretty clear. If this list sounds familiar, it's a very strong clue.
- Morning Agony: That sharp, stabbing pain in your heel as soon as your feet hit the floor.
- Pain After Rest: The pain might fade a bit as you get moving, but it comes roaring back after you’ve been sitting or standing in one place for a while.
- Post-Activity Ache: You often feel the worst of it after a workout or a long shift, not necessarily during.
- Heel Tenderness: The spot right in front of your heel bone is often sore if you press on it.
This creates a frustrating loop: you rest to feel better, but the pain just comes back with a vengeance when you move again. Recognizing these classic signs is crucial. To get a deeper understanding, check out our guide on what is plantar fasciitis. Knowing exactly what you're up against is half the battle.
How Your Job and Daily Habits Worsen Heel Pain
While we can point to the plantar fascia as the anatomical source of the pain, it's our daily lives that really set the stage for the problem. The job you do, the shoes you choose, and your own unique body mechanics can quickly turn a minor ache into chronic heel pain after standing all day. Getting to the bottom of these factors is the only way to find a solution that actually lasts.
It’s no surprise that jobs requiring long hours on your feet are notorious for causing foot problems. Think about it: nurses, teachers, retail workers, and construction crews all share a common enemy. Hard, unforgiving surfaces. Standing for eight hours straight on concrete is a world away from standing on a soft carpet or a cushioned mat.
Those hard floors offer absolutely zero shock absorption. This means your feet are forced to bear the full brunt of your body weight with every tiny movement. This constant, low-level trauma is one of the biggest triggers for inflammation in the plantar fascia.
Occupations at Highest Risk
Some jobs are just brutal on the feet. For healthcare professionals like nurses and doctors, the risk of developing plantar fasciitis is incredibly high. They pull grueling 8 to 12-hour shifts, almost entirely on their feet, which often leads to chronic pain that can seriously affect their work and well-being.
In fact, one study found that a staggering 83% of plantar fasciitis cases occur in active, working adults between the ages of 25 and 65. You can read more about these workplace findings and how they impact healthcare workers in particular.
Your job might have a strict dress code, but settling for unsupportive footwear is a fast track to foot pain. Shoes that are completely flat, flimsy, or have no real arch support force your plantar fascia to work overtime, straining it with every single step.
This is exactly why we have to look at the environmental and personal pieces of the puzzle. It’s not just about the pain itself; it’s about figuring out what’s causing it.
Personal Factors That Increase Your Risk
Beyond your job, a few personal factors can make you more likely to develop heel pain. These can act alone or team up to put even more stress on your feet.
- Body Weight: Every extra pound you carry adds a surprising amount of pressure to your plantar fascia. The good news is that even a small amount of weight loss can make a huge difference in reducing that strain.
- Foot Structure: The natural shape of your foot plays a massive role. Both flat feet (overpronation) and unusually high arches can mess with your gait, distributing weight unevenly and putting extra stress right on the heel.
- Age: As we get older, the natural fat pad in our heel that acts as a cushion starts to thin out. This reduces our foot’s built-in shock absorption, leaving us more vulnerable to pain.
- Improper Footwear: This is a big one. Shoes with weak arch support, worn-out soles, or a design that squeezes your feet will force them into unnatural positions, directly contributing to heel strain.
By figuring out which of these factors might be affecting you, you can start putting together a plan that targets the real issues. It’s all about addressing the root causes, not just chasing the symptoms.
Stretches You Can Do Right Now for Heel Pain
When your heels are aching after a long day on your feet, you need relief, and you need it fast. The good news is, you don't have to wait. A few simple, targeted stretches can work wonders to release the tension that's built up in your lower legs and feet.
It helps to think of your calf muscles and your plantar fascia as a single, connected chain. When your calves get tight from hours of standing, they pull on the Achilles tendon. This, in turn, tugs on your heel bone and puts a ton of strain on your plantar fascia. Stretching breaks this painful cycle. It's your secret weapon for both immediate comfort and long-term prevention.
Simple Stretches You Can Do Anywhere
You don't need a gym or any special equipment for these. You can do them at home, on a break at work, or as soon as you get home from your shift. The real trick is consistency, so try to make them a daily habit.
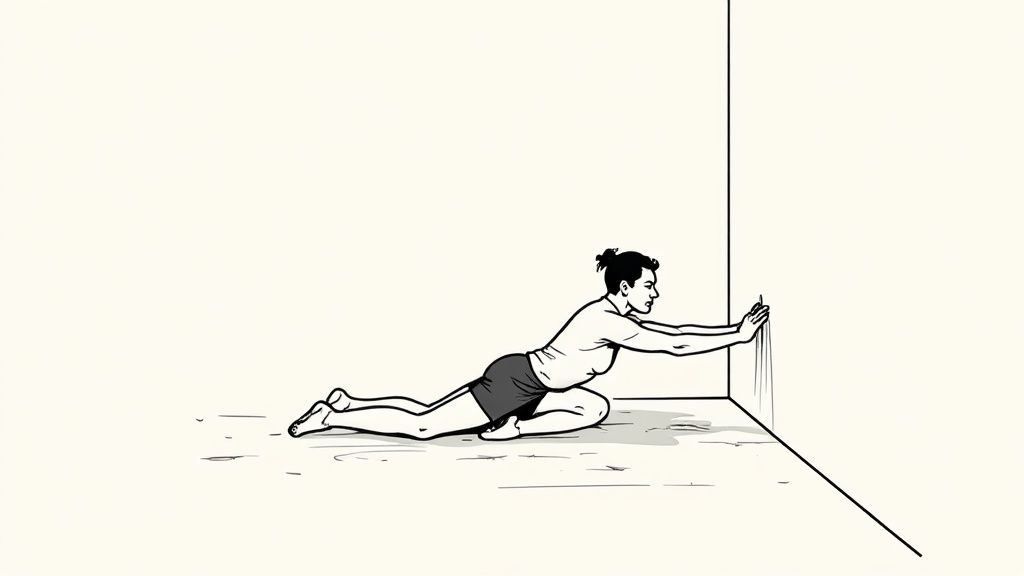
1. Standing Calf Stretch This is the classic for a reason. It goes right after the tight calf muscles that are often the root cause of heel pain.
- Find a wall and stand facing it, placing your hands on it for balance.
- Step one foot back, keeping the leg straight and your heel flat on the floor.
- Now, lean into the wall by bending your front knee. You should feel a nice, steady stretch in the calf of your back leg.
- Hold it for 30 seconds—no bouncing! Then, switch legs. Do this three times on each side.
2. Plantar Fascia Towel Stretch This one is a lifesaver, especially if you get that sharp, stabbing pain first thing in the morning.
- Sit down on the floor and extend your legs straight out.
- Grab a towel (or a resistance band if you have one) and loop it around the ball of one foot.
- Keeping your knee straight, gently pull the towel toward your body. You'll feel the stretch in your arch and calf.
- Hold for 30 seconds, and repeat three times on each foot.
A quick word of advice: A stretch should feel like gentle tension, not sharp pain. If you feel any pain, ease up a bit. Listening to your body is the key to getting relief safely.
Easy Self-Massage for Quick Relief
Stretching is fantastic, but adding a little self-massage can really take the edge off. These techniques are perfect for the end of a long day when your feet are tired and sore.
- Frozen Water Bottle Roll: This is a classic for a reason. Just freeze a regular water bottle, then sit down and roll it under your foot from heel to toe for 5-10 minutes. The cold tackles inflammation while the rolling motion massages that sore tissue.
- Tennis Ball or Lacrosse Ball Roll: For a deeper massage, grab a tennis ball (for a gentler touch) or a lacrosse ball (for more intensity). While seated, roll the ball under your foot, pausing to apply gentle, steady pressure on any particularly tender spots.
Think of these simple exercises as your first line of defense. By making them part of your daily routine, you can actively fight back against the strain, improve your flexibility, and finally get the comfort you've been looking for.
Finding the Right Shoes and Insoles for All-Day Comfort
Your shoes are your first, and most important, line of defense against heel pain after standing all day. Think of them like the foundation of a house. If that foundation is weak or cracked, the whole structure on top—your ankles, knees, hips, and back—will eventually start to feel the strain.
Just grabbing any old pair of shoes won't cut it. You have to know what to look for, seeking out specific features that deliver real, lasting support. The mission here isn't just to cover your feet, but to truly protect them from the relentless pounding they take on hard floors hour after hour.
What to Look for in a Supportive Shoe
Finding a genuinely supportive shoe has less to do with brand names or price tags and more to do with its actual construction. A shoe built for all-day standing will have a few key features that work together to cradle your foot and soak up impact.
Here’s what you should be looking for:
- Strong Arch Support: Your arch is your foot’s built-in shock absorber. A shoe that supports it helps spread your body weight evenly, taking a massive amount of stress off your plantar fascia.
- Deep Heel Cushioning: A well-cushioned heel cup is non-negotiable. It absorbs the jarring impact that shoots up your leg every time your foot hits the ground, protecting the sensitive fat pad under your heel.
- A Firm, Sturdy Structure: Try this: grab a shoe and try to twist it like a wet towel. If it bends and twists easily in the middle, it’s not supportive enough. A good shoe provides a rigid platform that prevents your foot from rolling inward or outward (overpronation), which is a major cause of heel strain.
- Wide Toe Box: Your toes weren't designed to be squished together. They need space to splay out naturally as you stand and walk. A cramped toe box can throw off your entire gait and lead to pain.
Quick tip: The right shoe should feel good the moment you put it on. That whole "break-in period" is often just a sign that your foot is being forced into a shape it doesn't like, which is a recipe for trouble.
To make it even clearer, here’s a quick comparison to help you spot the features of a great work shoe versus one that will cause pain.
Supportive vs Unsupportive Shoe Features
| Key Feature | What to Look For (Supportive) | What to Avoid (Unsupportive) |
|---|---|---|
| Midsole Stability | Firm and resistant to twisting. | Bends and twists easily in the middle. |
| Heel Counter | Stiff and structured to grip your heel. | Soft, flimsy, and easily collapsible. |
| Arch Support | Noticeably present and matches your arch. | Flat inside with no discernible support. |
| Toe Box | Roomy enough for toes to wiggle freely. | Narrow, pointed, or constricting. |
| Cushioning | Responsive foam that absorbs impact. | Thin, hard material that feels flat. |
Looking for these key differences when you shop can save you from months of unnecessary pain.
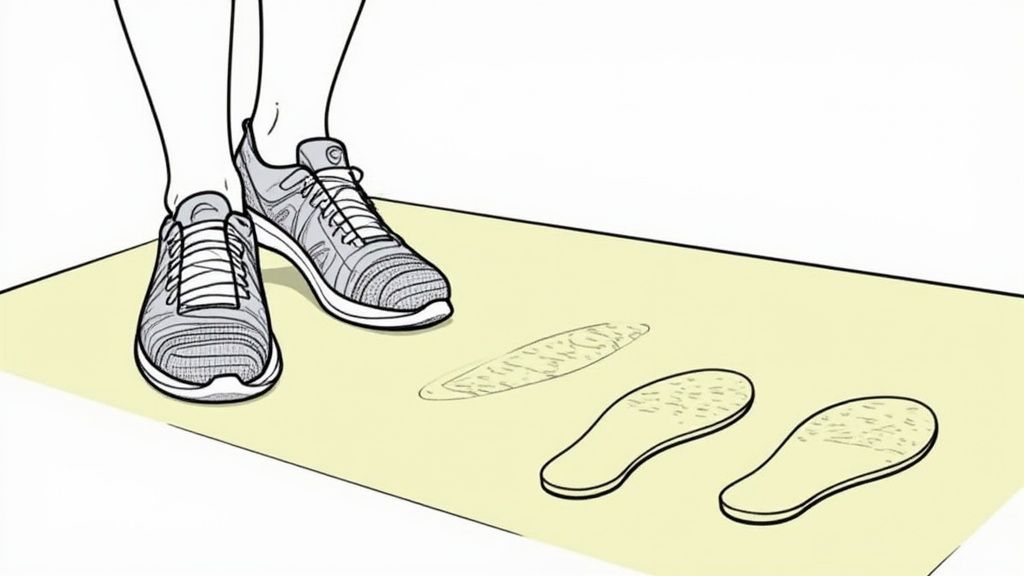
The Role of Insoles in Customizing Your Comfort
Even a fantastic shoe might not perfectly match your foot's unique contours. That’s where insoles come in—they are the ultimate upgrade, turning a pretty good shoe into your perfect shoe. They deliver targeted support exactly where you need it most.
Insoles are especially helpful if you have a specific foot type that makes you prone to heel pain, like flat feet or very high arches. By correcting those little biomechanical imbalances, they help keep your foot properly aligned and cushioned all day long.
You’ll find a ton of options out there, from basic gel inserts at the pharmacy to custom-molded orthotics from a podiatrist. To get a better handle on what's right for you, our guide on how to choose shoe inserts breaks it all down. Making a smart choice here can be the difference between constant pain and blissful relief.
When Your Heel Pain Requires a Doctor's Help
While trying things at home is a great first step, some types of heel pain after standing all day are more than just a nuisance. They’re your body’s way of sending up a flare, signaling that it’s time to call in a professional.
Knowing when to switch from self-care to a doctor’s visit is key. If the pain is so bad it changes the way you walk, or if you’ve been diligent with home remedies for a few weeks with no improvement, it's time to make that appointment. Pushing through serious pain often leads to chronic problems that are much tougher to solve down the road.
Key Signs to See a Professional
Don't brush off your heel pain if it’s accompanied by any of the following symptoms. These are clear signs that something more serious might be going on, and you’ll want a proper diagnosis from a doctor or podiatrist.
- Numbness or Tingling: That "pins and needles" feeling in your foot is never normal and needs to be checked out.
- Intense Swelling or Bruising: If your heel or the surrounding area is badly swollen or discolored and ice isn't helping, that's a major red flag.
- Pain at Rest: A heel that throbs and aches even when you’re sitting down with your feet up is a definite cause for concern.
- Inability to Bear Weight: If you can't put weight on your foot or find yourself limping just to get around, a professional evaluation is a must.
When you see a doctor, they'll likely start with a physical exam and ask about your lifestyle and daily routine. From there, they might recommend more advanced options like physical therapy, specialized night splints, or even prescription-grade orthotics for more targeted support. If you want to dive deeper, you can learn more about how to treat a plantar fasciitis with a structured medical approach.
Still Have Questions? Let's Clear Things Up
Even with the best advice, it's natural to have a few lingering questions when you're trying to get rid of nagging heel pain. Getting straight answers can make all the difference. Let's tackle some of the most common things people ask when their feet are screaming at them after a long day.
Do Compression Socks Actually Work?
You bet they do. Think of compression socks as a helpful, gentle squeeze for your legs. This pressure helps improve blood flow and keeps swelling down, which are two of the biggest reasons your feet and heels feel so achy and heavy after you've been on them for hours.
For people who stand all day, graduated compression socks are the gold standard. They're designed to be tightest at the ankle and get looser as they go up your leg. This smart design helps push blood back up towards your heart instead of letting it pool in your feet, which is a game-changer for reducing soreness.
How Long Will It Take for My Heel Pain to Go Away?
This is the million-dollar question, and the honest answer is: it depends. The timeline really hinges on how severe the problem is and how committed you are to your recovery plan.
For many people, sticking to a routine of daily stretches, icing the sore spots, and consistently using good shoes with supportive insoles can bring noticeable relief in just a few weeks. But for stubborn, long-term cases of plantar fasciitis, it could take anywhere from six months to a year to get back to 100%. The key is to start treatment the moment you feel that first twinge of pain.
The worst thing you can do is try to "tough it out." Listening to your body and taking action early with rest, stretching, and the right insoles is your fastest route back to comfort. Ignoring the pain almost always makes the problem worse and the recovery much, much longer.
Are Anti-Fatigue Mats a Gimmick?
Not at all. If you work on your feet but stay in roughly the same spot, an anti-fatigue mat is one of the smartest purchases you can make.
These mats provide a soft, cushioned layer that forces your leg muscles to make tiny, almost unnoticeable adjustments to maintain balance. These "micro-movements" are fantastic because they keep your blood circulating and take a huge amount of pressure off your feet, knees, and even your lower back. It’s a simple way to fight the strain of standing on hard surfaces like concrete all day.
Don't let heel pain after standing all day run your life. The right support can completely change how you feel. See for yourself how the targeted design of Samurai Insoles delivers the relief you need to get through your day without pain. Find your perfect fit at Samurai Insoles.



