The main difference between orthotics and insoles is pretty straightforward: custom orthotics are prescribed medical devices made to fix specific foot problems, while over-the-counter insoles are all about general comfort and cushioning.
A good way to think about it is comparing prescription glasses to the reading glasses you can buy at a drugstore. One is for correcting a diagnosed vision problem, while the other offers a little help for a common issue. Your choice really boils down to whether you need to correct a medical condition or just want to make your shoes a bit more comfortable.
Understanding the Core Distinction
When you're looking for foot relief, it's easy to get tangled up in the terms "orthotics" and "insoles." People often use them as if they mean the same thing, but they serve completely different roles and are made in very different ways. Getting this distinction right is the first step toward finding relief that actually works.
An over-the-counter insole is a mass-produced insert you can grab off the shelf at a local pharmacy or shoe store. Its main job is to add a layer of cushioning and maybe a little bit of generic arch support. They can be great for easing general foot fatigue after a long day of standing or walking.
A custom orthotic, on the other hand, is a prescription medical device. It's built from a highly-detailed 3D scan or cast of your feet, ordered by a podiatrist to treat a diagnosed foot problem. The goal isn't just comfort; it’s functional correction.
Key Functional Differences
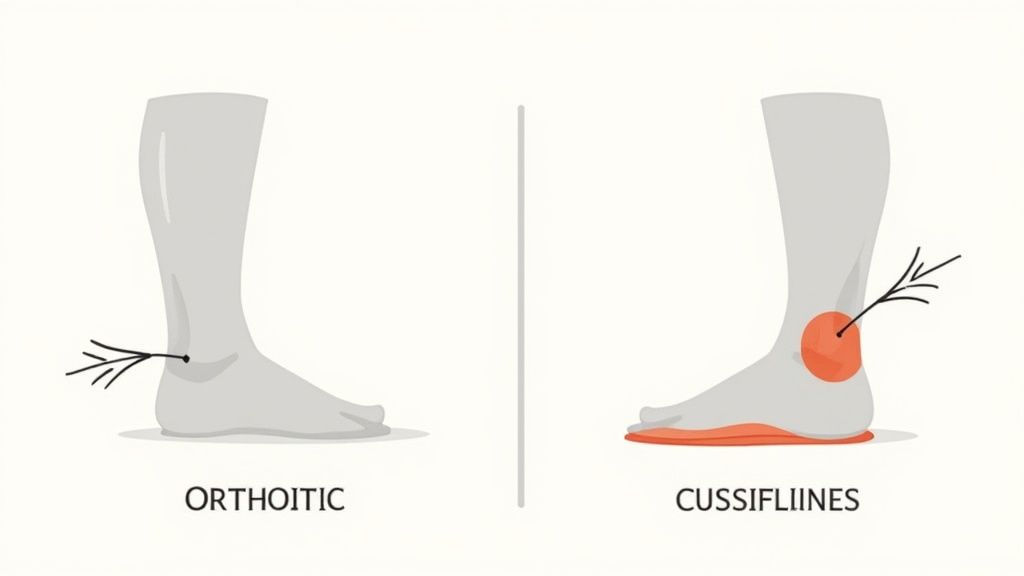
The real purpose of an orthotic is to guide your foot and ankle back into their most efficient alignment. It’s a tool for treating specific, diagnosed conditions.
- Custom Orthotics: These are engineered to correct problems like severe overpronation (what many call fallen arches), realign how your joints move, and support your foot’s unique structure.
- Over-the-Counter Insoles: These focus on absorbing shock and giving your foot a softer landing. This can certainly feel better, especially on hard floors, but it won't fix the root cause of a biomechanical issue.
The simplest way to frame the debate is this: An insole cushions the foot you currently have, while a true orthotic helps guide your foot toward a healthier alignment and function.
Quick Comparison: Orthotics vs. Insoles
To make things even clearer, let's break down the key differences side-by-side. This table gives you a high-level look at what separates a custom medical device from a standard shoe insert.
| Feature | Custom Orthotics | Over-the-Counter Insoles |
|---|---|---|
| Primary Purpose | Correct biomechanical issues | Provide cushioning and comfort |
| Creation Process | Custom-molded from a prescription | Mass-produced in standard sizes |
| Who Recommends It | Podiatrist or medical professional | Self-selected by the consumer |
| Typical Cost | High ($300 - $800+) | Low ($15 - $75) |
| Material | Rigid or semi-rigid medical-grade polymers | Foam, gel, or soft consumer materials |
| Lifespan | 2-5 years | 6-12 months |
As you can see, the investment, purpose, and creation process are worlds apart. One is a targeted medical treatment, while the other is a general-purpose comfort accessory.
The Role of Over-The-Counter Insoles
If you've ever walked down a pharmacy aisle, you've seen them: walls of over-the-counter (OTC) insoles. These are mass-produced inserts built to tackle one very common issue—general foot fatigue. They aren't medical devices; think of them more like comfort accessories for your shoes.
Their main job is to give you extra cushioning and absorb shock, which can make a huge difference when you're on your feet all day. It’s like adding a plush pillow-top to a firm mattress. This immediate comfort boost is their biggest selling point and a key difference when you're weighing orthotics vs. insoles.
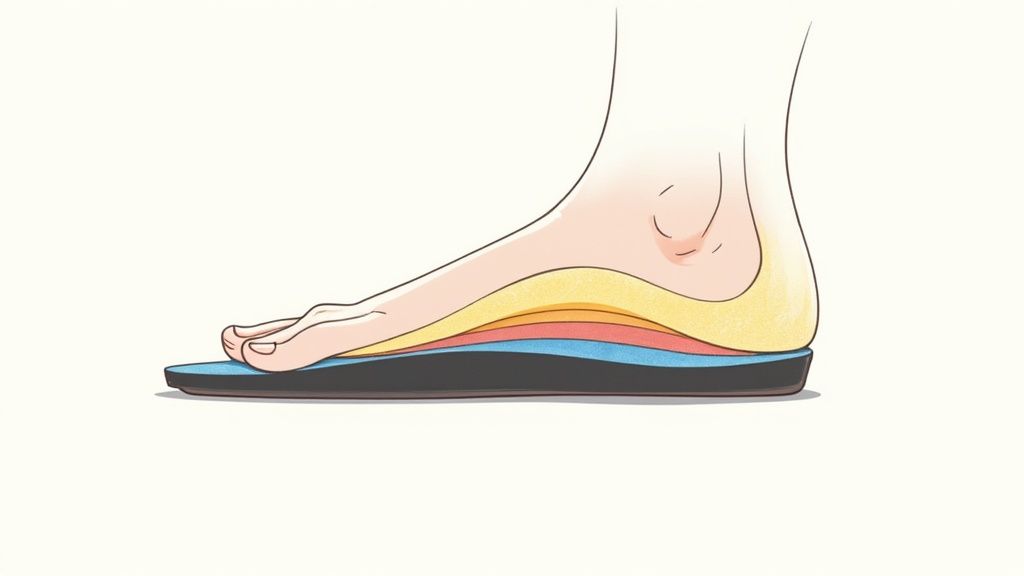
What Insoles Are Made Of
The materials in OTC insoles are all about immediate comfort and shock absorption. You'll generally run into two main types:
- Foam: Memory foam and similar polyurethane foams are incredibly common. They do a great job of molding to the basic shape of your foot, giving you a soft, cushioned feel that helps reduce pressure points.
- Gel: You’ll see gel pads and full-length gel insoles everywhere, and for good reason. They are fantastic at absorbing shock, especially if you spend a lot of time walking or standing on unforgiving surfaces like concrete.
While these materials feel great at first, they compress pretty quickly and offer next to no structural support. They simply weren't designed to fix how your foot is aligned or treat any deeper biomechanical problems.
An over-the-counter insole is a temporary fix for tired feet. It offers surface-level comfort but won’t get to the root cause of chronic foot pain or structural issues like overpronation.
When an Insole Is the Right Choice
So, when does grabbing a simple insole make sense? Imagine a retail worker who spends eight hours a day pacing on hard tile floors. They might not have a condition like plantar fasciitis, but by the end of the day, their feet are just plain sore.
In a situation like that, a gel or foam insole can be a game-changer. It absorbs the constant impact and adds a much-needed layer of cushioning. It's a simple, low-cost way to handle foot fatigue caused by your environment, not by an underlying medical issue.
If you have a more specific issue like heel pain, looking into insoles for plantar fasciitis can provide more targeted cushioning. But it's vital to know where they fall short.
These inserts are a fantastic tool for making shoes more comfortable, but they are absolutely not a replacement for medical treatment. If your pain is sharp, won't go away, or is tied to a structural problem, an insole will only cover up the symptoms. It won't fix the problem, and you might risk making it worse in the long run.
What Exactly Are Custom Orthotics?
While over-the-counter insoles are all about general comfort, custom orthotics are in a completely different league. Think of them as highly specialized medical devices, prescribed by a podiatrist to fix a diagnosed biomechanical problem in your feet. Their job isn't just to add cushioning—it's to correct how your foot functions. This corrective role is the single biggest difference when you compare them to basic insoles.
Unlike a generic insert you’d grab off the shelf, a custom orthotic is built from a precise, detailed map of your unique foot structure. The process usually involves a podiatrist taking a 3D scan or even a physical plaster cast of your feet. This captures every curve, arch, and contour, creating a blueprint for a device that can realign your foot and ankle to work more efficiently and reduce strain.
This is why they’re the go-to solution for more complex foot conditions. The market for foot support is clearly divided, with custom orthotics recognized for their clinical effectiveness in fixing specific issues. It's a world away from mass-produced comfort insoles.
From a Doctor's Diagnosis to a Finished Device
Getting custom orthotics is a true medical process from start to finish. It all begins with a podiatrist giving you a thorough biomechanical assessment. They’ll watch how you walk (your gait), check the mobility in your joints, and carefully analyze your foot's structural alignment. This deep dive helps pinpoint the root cause of your pain, whether it’s severe overpronation or an unusual walking pattern.
Once the problem is identified, a precise impression of your feet is taken. That mold is then sent off to a specialized lab where your orthotics are crafted from durable, medical-grade materials. The final step is a fitting with your podiatrist to make sure the device fits perfectly inside your shoes and to make any small adjustments needed for maximum comfort and effectiveness. You can learn more about how orthotic inserts make a difference right here in our guide.
A custom orthotic is engineered to do one specific job: correct your foot’s alignment and mechanics. It’s a therapeutic tool designed to address the underlying cause of conditions like diabetic foot ulcers or severe plantar fasciitis, not just mask the symptoms.
Types of Custom Orthotics and What They Do
Custom orthotics aren't a one-size-fits-all product. They come in several varieties, each built for a different purpose:
-
Rigid Orthotics: Often made from firm materials like carbon fiber or plastic, these are all about control. They’re designed to manage motion in the two major joints of your foot, making them fantastic for correcting alignment and easing pain that radiates up into the legs, thighs, and lower back.
-
Semi-Rigid Orthotics: These offer the best of both worlds, blending control with cushioning. By layering soft and firm materials, they provide dynamic balance and support, which is why they are often prescribed for athletes who need support that moves with them.
-
Soft (Accommodative) Orthotics: Built from soft, compressible materials, these are focused on comfort and protection. Their main job is to provide cushioning, absorb shock, and take pressure off painful spots. This makes them ideal for sensitive feet, especially for people with conditions like diabetic foot ulcers or severe arthritis.
A Detailed Comparison of Key Differences

So, you're trying to figure out what to put in your shoes—orthotics or insoles? It’s a common question, and getting it right is crucial for your comfort and foot health. Let's be clear: this isn't about one being "better" than the other. It's about which one is the right tool for your specific job.
To settle the "orthotics vs insoles" debate for yourself, you have to look past the marketing and get down to the brass tacks: what they do, what they're made of, how they're made, and what they cost. Let's break it down.
Purpose and Function
The biggest difference between the two comes down to their fundamental purpose. They're designed to do very different things.
Over-the-counter insoles are all about comfort and cushioning. Think of them as shock absorbers. Their job is to make your shoes feel softer and reduce that general achy feeling you get after a long day on your feet. They're perfect if you don't have a specific medical problem but just want a little extra padding.
Custom orthotics, on the other hand, are about correction and control. These are medical devices, pure and simple. They're prescribed by a professional to fix a problem, like realigning your foot to combat severe overpronation or providing targeted support for a diabetic foot. They don't just cushion your foot; they actively change how it functions.
You could say an insole cushions the foot you have, while an orthotic helps create the foot you need for proper alignment and function.
Material and Durability
The stuff they're made of directly affects how they perform and how long they'll last. And believe me, the difference is night and day.
- Over-the-Counter Insoles: You'll usually find these are made from consumer-grade materials like soft foam or gel. They feel great right out of the box, but that plush comfort comes at a price—they compress and wear out pretty quickly.
- Custom Orthotics: These are built to last, using durable, medical-grade materials like rigid polypropylene, semi-rigid graphite, or specialized foams. These materials are chosen specifically for their ability to provide consistent structural support day after day, year after year.
Because of this, you’ll likely need to replace your off-the-shelf insoles every 6-12 months. A well-made custom orthotic, with proper care, can serve you well for 2 to 5 years, sometimes even longer.
Customization and Fit
Here’s where the two paths really diverge. One is a one-size-fits-most solution, while the other is made just for you.
OTC insoles are mass-produced based on shoe size. Sure, you can often trim them down with a pair of scissors to fit the length of your shoe, but that’s it for customization. The arch shape is generic, so it might be a perfect match for your foot, or it might not. It's a bit of a gamble.
Custom orthotics are the complete opposite. They are created from a precise 3D scan or plaster mold of your actual feet. This process captures every nuance of your foot's structure—your specific arch height, your foot's unique shape, and any biomechanical quirks. That "glove-like" fit is what allows them to provide the targeted correction needed for medical issues.
To give you a clearer side-by-side view, let's put these features into a table.
Detailed Feature Showdown: Orthotics vs. Insoles
This table breaks down the key attributes head-to-head, helping you see exactly where the value lies for each option.
| Attribute | Custom Orthotics | Over-the-Counter Insoles |
|---|---|---|
| Intended Purpose | Corrects specific biomechanical issues and treats medical conditions. | Provides general comfort, cushioning, and shock absorption. |
| Creation Process | Created from a 3D scan or plaster cast of your feet. | Mass-produced in standard shoe sizes; may be trimmable. |
| Materials Used | Medical-grade polypropylene, graphite, or high-density foams. | Consumer-grade gel, soft foam, or basic plastic. |
| Level of Support | Firm and corrective, designed to realign your foot. | Soft and flexible, designed for padding and comfort. |
| Durability/Lifespan | 2 to 5+ years with proper care. | 6 to 12 months on average. |
| Typical Cost | $300 - $800+ | $15 - $75 |
| Best For | Diagnosed conditions like plantar fasciitis, severe pronation, diabetic foot care. | Minor foot fatigue, adding cushioning to shoes, standing for long hours. |
As you can see, the choice isn't just about price—it's about investing in a solution that matches the complexity of your needs.
Cost and Lifespan
Finally, let's talk about the money. The price difference between orthotics and insoles is significant, but you have to look at it as an investment in your health and comfort.
An over-the-counter insole is an easy, low-cost buy, usually running between $15 and $75. This makes them a great, accessible starting point if you're just looking for a bit more comfort. But remember, with their shorter lifespan, those replacement costs will add up over the years.
Custom orthotics are a serious medical purchase, often costing anywhere from $300 to $800. That high upfront price tag can be intimidating, but it covers the podiatrist's expertise, the detailed casting or scanning process, and the manufacturing of a durable medical device built to last. When you factor in their longevity and corrective power, you're getting significant long-term value.
When Is an Insole the Right Choice for Foot Pain?
So, how do you know if you should grab an over-the-counter insole or see a specialist for a custom orthotic? It really boils down to one simple question: are you trying to manage a diagnosed medical condition, or are you just looking for more comfort in your day-to-day life?
For most people dealing with tired, achy feet, a high-quality insole is the perfect starting point. It’s a practical, immediate way to get relief without the cost and hassle of a medical appointment.
Look for These Telltale Signs
Think about the specific moments your feet start to hurt. If your pain is situational—tied to what you’re doing or where you’re standing—an over-the-counter insole is likely what you need.
- You're on your feet all day: Teachers, nurses, and retail staff know this pain well. Standing for 8+ hours on hard floors is brutal. A good insole adds the cushioning and support your shoes are missing, absorbing that constant shock.
- Your favorite shoes don't fit quite right: We all have that pair of shoes that's just a bit too loose. An insole can fill that extra space, giving you a snugger fit and stopping your foot from sliding around, which prevents blisters and instability.
- You're an athlete who needs better shock absorption: Runners and basketball players pound the pavement, and their feet pay the price. A performance-minded insole can dramatically reduce the jarring impact on your joints during intense activity.
- You're dealing with temporary soreness: Maybe you walked all over a new city on vacation or pushed it a little too hard on a hike. For that occasional, non-chronic ache, a comfortable insole gives your feet the TLC they need to recover.
In these situations, the goal isn't to fix a deep-seated biomechanical problem. It's about adding a layer of support and comfort that your shoes just don't provide on their own.
An over-the-counter insole is the right tool when your foot pain is a reaction to your environment or activity, not the result of a diagnosed, underlying condition.
Finding the Sweet Spot Between Basic Inserts and Custom Orthotics
Sometimes, those flimsy gel or foam inserts you find at the drugstore just don’t cut it. But the thought of shelling out for expensive custom orthotics feels like way too much. This is exactly where podiatrist-designed insoles like Samurai Insoles shine. They're built to give you medical-grade support without the prescription and the hefty price tag.
Take the Samurai Insoles Ninjas, for example. They have a springy, structured design that’s thin enough to slip right under your shoe’s existing liner, providing targeted support to combat overpronation. If you need more pillowy softness, the Sumos model adds an extra layer of foam for fantastic shock absorption.
These aren't your average drugstore inserts. They offer proven, targeted relief, making them a smart upgrade when you need something more substantial but aren't quite ready for a fully custom device.
When a Custom Orthotic Becomes Necessary
While a good over-the-counter insole can be a lifesaver for everyday aches, there are definite times when you need to call in the professionals. Knowing when to make that call is a huge part of the orthotics vs. insoles conversation, because picking the wrong one can mean you’re just delaying real treatment.
Think of it this way: when your foot pain shifts from a mild annoyance to a chronic, daily battle, it’s probably time to see a podiatrist. An insole is great for temporary soreness, but a custom orthotic is a medical device designed to correct an underlying issue. If your pain is sharp, stubborn, and doesn't ease up after a few weeks of rest and using quality insoles, your feet are telling you they need more help.
Structural Issues and Chronic Conditions
Some foot problems are simply too complex for a one-size-fits-all solution. In these cases, a professional diagnosis and a custom-built device are almost always the right move.
- Significant Biomechanical Problems: If you have severe overpronation (your ankle collapses inward) or supination (it rolls outward), a generic insole just can't provide the targeted correction needed. A podiatrist will design an orthotic to physically realign your foot’s movement.
- Structural Foot Deformities: Conditions like unusually high arches, rigid flat feet, or bunions that throw off your gait often require the kind of precise, firm support that only a custom orthotic can deliver.
- Chronic Medical Conditions: People with diabetes or arthritis face unique challenges. Custom orthotics are built to redistribute pressure away from sensitive areas to prevent diabetic ulcers or to cushion and support painful, arthritic joints in ways a simple insert cannot.
Another clear sign is persistent nerve pain. Our guide to understanding Morton's Neuroma and finding relief goes into more detail, but this type of pain is a definite signal to seek professional evaluation.
Here's the bottom line: if your foot pain stems from a structural problem or a diagnosed medical condition, a custom orthotic isn't just an upgrade—it's an essential part of your treatment.
This growing understanding of specific foot health needs is why the foot care industry is booming. The global orthotic insoles market was valued at USD 3.36 billion in 2022 and is expected to grow dramatically. Much of this is driven by people seeking real, preventive solutions for conditions like plantar fasciitis and flat feet, which often require more than just basic cushioning. You can discover more about these market insights on futuremarketinsights.com.
Ultimately, if you’ve already tried quality insoles, supportive shoes, and rest but are still in pain, your body is sending a clear message. Listen to it. Seeking a professional opinion is the most important step you can take toward finding lasting relief.
Common Questions About Orthotics and Insoles
When you’re trying to decide between orthotics and insoles, a few practical questions almost always pop up. Getting clear answers to these can make all the difference in choosing confidently and getting the relief you need.
How Long Do They Last?
Durability is one of the biggest distinctions between the two. Think of custom orthotics as a long-term investment. Because they’re built from tough, medical-grade materials, you can expect them to last anywhere from 2 to 5 years.
Over-the-counter insoles, on the other hand, are made from softer materials like foam or gel. They’re designed for comfort, not longevity, so they usually wear out much faster. You'll likely need to replace them every 6 to 12 months.
Do They Need a Break-In Period?
Absolutely, especially for custom orthotics. Your body needs time to adjust to the new support and alignment. It's a good idea to start by wearing them for just a couple of hours a day, then gradually work your way up over a week or two.
Most basic insoles feel comfortable right out of the box and don't require much, if any, break-in time.
A crucial takeaway is that while orthotics and insoles are excellent for foot-specific discomfort, it's also helpful to be aware of a wider range of natural chronic pain relief methods for overall well-being. This broader perspective can support your journey toward a pain-free life.



