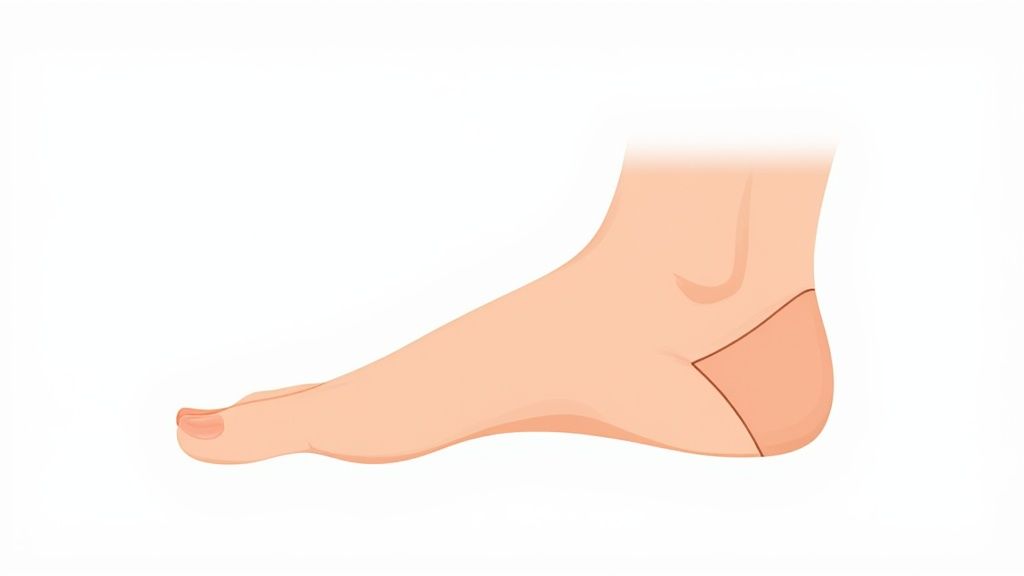
When the arch of your foot collapses and the entire sole makes contact with the ground, you're dealing with what's known as fallen arches, or pes planus in medical terms. The best way to think about your foot's arch is like a natural suspension bridge, engineered to distribute your body weight and absorb the shock of every step.
But when the primary supports for that bridge—your tendons and ligaments—start to weaken, the whole structure sags. This is what most of us call having flat feet.
What Are Fallen Arches and Why Do They Happen?
Fallen arches are pretty common, but the reasons behind them are surprisingly diverse. It's rarely just one single thing that causes this change in your foot's anatomy. More often than not, it's a mix of your genetics, your lifestyle, and your overall health coming together. Getting to the root of the "why" is the first real step toward finding relief that actually works.
For a lot of people, the tendency for flat feet is something they were born with. Some of us just have looser ligaments and more flexible joints, which means a well-defined arch might never form in the first place. In fact, it's perfectly normal for babies and toddlers to have flat feet. Most kids develop their arches by the time they're 10, but for 15% to 25% of the population, this flexible flatfoot condition sticks around into adulthood.
The Main Triggers for Fallen Arches
Genetics aside, plenty of things can cause a perfectly good arch to collapse over time. This is what's often called "adult-acquired flatfoot," where a previously normal arch gives way due to new stresses or underlying health problems.
One of the biggest culprits is simply the wear and tear that comes with getting older. The posterior tibial tendon, which is the main tendon propping up your arch, can get stretched out, weakened, or even torn after years of use. Think of it like an old rubber band that’s lost all its snap.
Certain life events and health issues can also put you on the fast track to fallen arches:
- Significant Weight Gain: Carrying extra weight puts a tremendous amount of continuous pressure on your feet. That constant strain can make the supporting structures more likely to give out.
- Repetitive Impact: High-impact activities like running or jobs that keep you on your feet all day can lead to cumulative damage to the tendons and ligaments.
- Traumatic Injury: A sudden, sharp injury from a fall or an accident can knock bones out of place or tear tendons, causing the arch to collapse almost instantly.
- Health Conditions: Diseases like rheumatoid arthritis and diabetes can directly harm tendon health and nerve function, effectively weakening the foot's natural support system from the inside out.
A key marker that professionals use to assess flat feet is the height of the navicular bone, a crucial bone right in the middle of your arch. Where this bone sits is determined by a mix of factors, from your genetics and body weight to how active you are and even the shoes you wear. You can explore more research on arch evaluation in young adults to see how it's measured.
Quick Overview of Fallen Arch Causes
To make sense of all these moving parts, it's helpful to group the causes into a few main categories. The table below offers a simple breakdown of the main reasons people develop fallen arches, helping you quickly identify the potential source.
| Cause Category | What It Means | Who It Typically Affects |
|---|---|---|
| Congenital | You were born with it, usually due to genetics or loose ligaments. | Children and adults who never really developed a high arch. |
| Acquired | A normal arch collapses later in life due to stress, injury, or aging. | Adults, often triggered by weight gain, overuse, or an injury. |
| Secondary | Flat feet show up as a side effect of another medical issue. | People with arthritis, diabetes, or nerve-related disorders. |
By grasping these fundamental causes, you can start to see how different factors work together to affect your foot health. This knowledge is key to recognizing the signs early and finding the right kind of support.
A Look Inside Your Foot's Arch Structure
To really get what’s happening with fallen arches, we need to pop the hood and look at the brilliant engineering inside your foot. It's not just a solid block you stand on; it’s a complex, dynamic machine built to handle incredible forces every single day.
At the core of this machine are the arches. Most of us think of the foot as having just one arch, but there are actually three distinct arches working in concert. Together, they form a strong, flexible, triangular dome that absorbs shock every time you take a step, jump, or even just stand. This clever design is what distributes your body weight evenly across your feet and up your legs.
The Three Arches of Your Foot
Think of a tripod—it's incredibly stable because it has three points of contact with the ground. Your foot’s arches create a similar foundation, giving you balance and support.
-
The Medial Longitudinal Arch: This is the one everyone knows. It’s the high, curved arch running along the inside of your foot, from your heel to the ball. Consider it the main spring, absorbing the bulk of the impact when you move.
-
The Lateral Longitudinal Arch: Running parallel to the big arch but on the outside of your foot, this one is much lower and flatter. Its main job is to provide stability and help balance your weight as it shifts.
-
The Transverse Arch: This arch runs from side to side across the midfoot, just behind the ball. It creates a dome shape that helps distribute pressure across the front of your foot.
This trio of arches is formed by the tarsal and metatarsal bones, all strapped together by a tough web of ligaments. But this bony framework, while strong, can't hold its shape under load without some help. That's where a very important tendon comes into play.
The Most Important Support Cable
While bones and ligaments provide the static structure, the tendons are what provide active, dynamic support. When it comes to holding up your arch, the posterior tibial tendon is the star of the show.
Think of the posterior tibial tendon as the main suspension cable on a bridge. It runs from a muscle in your calf, down the inside of your ankle, and attaches to several bones on the underside of your foot. Its job is to actively hoist the arch up, keeping it taut and supported with every step.
When this tendon is healthy, your arch stays strong and does its job. But if the posterior tibial tendon gets overworked, stretched out, inflamed, or torn, it starts to fail. The "suspension cable" goes slack, and the entire arch structure begins to sag and flatten. This problem, known as posterior tibial tendon dysfunction (PTTD), is one of the leading causes of adult-acquired flatfoot.
Once you understand this interplay between the bones and the soft tissues holding them up, it all starts to make sense. Fallen arches aren't usually a bone problem; they're a failure of the support system that's supposed to maintain your foot's incredible architecture.
The Hidden Factors That Increase Your Risk

While the anatomy of a fallen arch is pretty clear, what causes it to happen is usually a mix of different things. It’s rarely one single event. More often, it's a combination of factors that, over time, put your arches under more stress than they can handle. Getting a handle on these risk factors is the first step toward protecting your feet for the long haul.
A good way to think about your foot’s arch is to picture a small, flexible bridge. This bridge is built to support a certain amount of weight and stress. But various life events and health issues can either weaken the bridge's structure or pile on way more traffic than it was designed for. When the load is constantly too heavy, the bridge starts to sag and, eventually, it can collapse.
The Impact of Age and Body Weight
Two of the biggest players here are simply getting older and the amount of weight our feet have to carry every single day. As we age, our tendons—especially the posterior tibial tendon that does the heavy lifting for the arch—naturally start to lose some of their strength and springiness. This gradual weakening makes them much more vulnerable to strain from just walking around.
At the same time, any extra body weight puts a huge, constant force on this already aging support system. For every extra pound you carry, your feet feel several pounds of pressure with each step. That relentless load can really speed up the wear-and-tear, stretching out the ligaments and tendons until they just can't hold the arch up anymore.
A 2020 study really highlights this connection, finding that 51.6% of patients with hypertension also had flat feet. The research showed a clear link between a higher Body Mass Index (BMI) and flatter arches, even in people who weren't considered obese. You can discover more insights about the link between BMI and foot health in the full study.
This one-two punch of weakening support and increasing load creates the perfect storm for developing what's known as adult-acquired flatfoot. It’s also why a collapsing arch can cause your ankle to roll inward, a common problem called overpronation. If you think that sounds familiar, you can learn more about what overpronation of the foot is and how it all connects.
Lifestyle and Occupational Stresses
What you do every day matters, too. Your job and hobbies can put a ton of repetitive stress on your feet, pushing your arches to their limit day in and day out.
Just think about these common situations:
- High-Impact Activities: Sports like running, basketball, or tennis involve constant pounding on hard surfaces. This can easily lead to tiny tears and inflammation in the tendons supporting your arch.
- Prolonged Standing: If your job requires you to be on your feet for hours—like in nursing, retail, or construction—your arches are under continuous strain with very little chance to rest and recover.
Underlying Health Conditions
Finally, some health conditions can go on the attack, directly weakening the very structures that support your feet. When this happens, fallen arches can be a secondary result of a bigger issue.
Three of the most common culprits are:
- Rheumatoid Arthritis: This autoimmune disease causes joint inflammation, which can badly damage the small joints in your feet and weaken the ligaments and tendons around them.
- Diabetes: When poorly managed, diabetes can cause nerve damage (neuropathy) and reduce sensation in the feet. It also affects blood flow, which is critical for keeping your tendons healthy and strong.
- Pregnancy: During pregnancy, the body releases a hormone called relaxin to loosen ligaments for childbirth. This can also affect the ligaments in your feet, sometimes leading to a temporary or even permanent collapse of the arches.
When you connect all these dots—genetics, age, weight, activities, and your overall health—it becomes much clearer how they all play a role in the stability, or instability, of your arches.
How to Spot the Symptoms of Fallen Arches

It’s surprisingly common for people to have fallen arches without ever knowing it, especially when the change happens over years. The symptoms can be sneaky, starting as a small annoyance that you brush off, but gradually growing into a constant ache. Learning to spot these early clues is the best way to get ahead of the issue before it starts getting in the way of your life.
The most obvious sign is visual—when you stand up, your entire foot sole makes contact with the floor. But often, the symptoms of a collapsing arch are felt long before they're seen.
Think of your arches like the suspension system in a car. When the suspension is shot, you start feeling every single bump in the road. In the same way, when your arch fails, your body starts feeling the impact of every step.
Where Does It Hurt?
Pain is your body's check-engine light, and with fallen arches, it can flash in a few different places. Since the arch isn't doing its job of absorbing shock, that stress has to go somewhere.
You’ll most likely feel it in these spots:
- Your Heels and Arches: This is the classic complaint. It might be a dull, throbbing ache that sticks around after a long day, or it could feel like a sharp, stabbing pain when you first get out of bed.
- Swollen Ankles: Look for swelling on the inside of your ankle. This is often a sign that the posterior tibial tendon, the primary support structure for your arch, is overworked and inflamed.
- Tired, Achy Feet: Do your feet just feel exhausted, heavy, or sore after what feels like very little effort? That's because the muscles are struggling to pick up the slack from your collapsing arch.
The most important thing to understand is that the pain often doesn't stop at your feet. An unstable arch throws off your body's entire alignment, which can lead to aches and pains in your shins, knees, hips, and even your lower back. It’s your body's way of telling you that the foundation is shaky.
Other Telltale Signs to Look For
Pain is a big one, but it’s not the only symptom. The physical change in your foot's structure can cause other problems that might not seem connected at first glance.
Be on the lookout for these other clues:
- Your Feet Have Changed Size: As your arch flattens, your foot actually lengthens and widens. You might even find yourself needing to go up a shoe size.
- You Walk Differently: Have you noticed your ankles caving inward when you walk? This is called overpronation, and it often causes the inner edge of your shoes to wear down much faster than the outside.
- Standing on Your Tiptoes is Tough: If the posterior tibial tendon is weak, you'll find it difficult to lift your heels and stand on the balls of your feet.
Recognizing these signs is the first step toward getting things sorted. If this sounds a lot like what you’re experiencing, our guide to fallen arches symptoms, causes, and treatment offers a much deeper dive. The sooner you identify the problem, the sooner you can find the right support and stop chronic pain from affecting your balance and mobility.
How a Doctor Figures Out If You Have Flat Feet
If you've been dealing with nagging foot pain or you've noticed your arches just aren't what they used to be, seeing a podiatrist or orthopedic specialist is a great idea. They can get to the bottom of what's going on. The whole process of getting a diagnosis is actually pretty straightforward, so there's no need to feel nervous about the appointment.
First things first, your doctor will want to see how your feet behave—both when you're standing still and when you're moving around. This initial hands-on check-up usually gives them almost all the information they need.
The Physical Exam
During the physical exam, the doctor will watch you stand and walk. This is where the classic signs of fallen arches really show themselves, as your body weight puts pressure on your feet. It's a simple but incredibly effective way to see your foot's mechanics in action.
Here are a few things the doctor will be on the lookout for:
- Your Shoe Wear Patterns: They'll probably ask to see the shoes you wear most often. If the inner side of the sole is worn down way more than the rest, that’s a dead giveaway for the kind of overpronation that comes with flat feet.
- The "Too Many Toes" Sign: This one sounds a little funny, but it's a real diagnostic clue. When looking at your heels from behind, a doctor should only see your pinky and fourth toe. If they can see more, it means your foot is rotating outward, which often happens when an arch collapses.
- Flexibility and Movement: The doctor will also move your foot and ankle around to test its flexibility. This helps them tell the difference between a flexible flatfoot (where you have an arch when you're sitting but it disappears when you stand) and a rigid flatfoot (where the foot is flat all the time).
This part of the exam helps the doctor gauge how severe the issue is and find any sore or swollen spots, especially around the posterior tibial tendon, which is a common culprit.
A big piece of the puzzle is figuring out why your feet are flat. The doctor needs to know if this is something you've had your whole life that's just now causing pain, or if it's an "acquired" issue that developed later due to an injury or a problem with a tendon.
When Imaging Tests Come into Play
Most of the time, the physical exam tells the doctor everything they need to know. But every so often, they'll want a closer look at the bones and soft tissues inside your foot. If they think something more complicated is going on, like a torn tendon or a bone alignment issue, they'll order an imaging test.
These are the most common ones:
- X-rays: These are fantastic for looking at the bones. An X-ray can quickly show if you have a fracture, dislocation, or arthritis that might be contributing to your flat feet.
- MRI (Magnetic Resonance Imaging): If the doctor is worried about a tendon or ligament, an MRI is the way to go. It gives incredibly detailed pictures of soft tissues, making it easy to spot things like inflammation or tears in the posterior tibial tendon.
You won't always need these tests, but when you do, they give your doctor a complete picture to build the best possible treatment plan just for you.
Effective Strategies to Manage and Support Your Arches
So, you've learned you have fallen arches. The next logical question is, "What do I do now?" The great news is you don't have to jump straight to drastic measures. There are plenty of practical, non-surgical ways to manage your symptoms and get back to living comfortably.
Think of it like this: your foot's natural support system is a bit like a sagging shelf. You can't just wish it back into place, but you can add strong brackets underneath to hold the weight. These management strategies are your brackets—they provide external support, help you strengthen your foot's internal structure, and involve making smarter daily choices to take the strain off.
The Foundation of Support: Shoes and Orthotics
The fastest way to feel a difference is by changing what you put on your feet. The right shoes and inserts are game-changers because they act as an external foundation, picking up the slack from your overworked tendons and ligaments.
Supportive shoes are your first line of defense. When you're shopping, look for shoes with a firm back part that cups your heel, a midsole that doesn't twist easily, and a nice, wide base. These features are designed to stop your foot from rolling inward too much (overpronation), which is a classic issue with fallen arches.
But the real secret weapon for many people is orthotic inserts. These aren't your average drugstore gel pads. A good orthotic is engineered to support your specific arch shape, guiding your foot back into a healthier alignment and absorbing the shock of each step. By creating this crucial scaffolding, orthotics can relieve pain not just in your feet, but all the way up your knees, hips, and back. You can learn more about the best orthotic insoles for fallen arches to see how they really work.
Fallen arches are incredibly common, affecting an estimated 20% to 37% of people worldwide. Research highlights a strong link to factors like a sedentary lifestyle and obesity. In fact, flat feet are the reason behind up to 90% of all foot-related doctor visits. If you're curious about the bigger picture, you can read more about these findings on global foot health.
Building Strength from Within Through Exercise
While orthotics give you immediate, external help, exercises work on building up your foot's own internal support system. By strengthening the muscles in your feet and lower legs, you create a stronger, more stable foundation from the inside out.
It's like reinforcing that sagging shelf from below with new, stronger pillars. These simple exercises are easy to do at home and can make a huge difference over time.
- Towel Curls: This one is a classic for a reason. Sit in a chair, place a small towel on the floor, and use just your toes to scrunch it up toward you. It's fantastic for targeting those small, deep muscles in your foot.
- Calf Stretches: When your calf muscles are tight, they can pull on your heel and make your arch collapse even more. To stretch them, face a wall, step one foot back, and lean forward until you feel a gentle pull in the calf of your back leg. Hold for 30 seconds, then switch.
- Arch Lifts: Whether you're sitting or standing, try to raise the arch of your foot while keeping your toes and heel on the ground. This move directly targets the muscles that hold up your arch.
With these exercises, a little bit every day goes a long way. When you combine this consistent strengthening with the instant support you get from good shoes and orthotics, you’ve got a powerful one-two punch for managing your fallen arches.
Common Questions About Fallen Arches
Even after digging into the causes and symptoms, you probably still have a few questions floating around. Let's tackle some of the most common ones we hear, giving you clear, practical answers to help you manage your foot health with confidence.
Can You Actually Reverse or Cure Fallen Arches?
For most adults who've developed fallen arches over time, the condition can't be fully reversed without surgery. It helps to think of the ligaments supporting your arch like a rubber band that's been stretched out for too long—they simply won't snap back to their original tightness on their own.
But that doesn't mean you're stuck with the pain. In fact, non-surgical treatments are fantastic for managing symptoms and keeping the problem from getting worse.
Key Takeaway: The goal of non-surgical management isn't to magically "cure" a flat foot but to support it. Things like orthotics, good shoes, and physical therapy are all designed to improve how your foot works and feels, even if they don't rebuild the arch itself. Surgery is typically only considered for severe cases when nothing else has brought relief.
Is It Safe to Exercise with Flat Feet?
Absolutely! Not only is it safe, but it's often highly recommended. The key is to be smart about it and take the right precautions so you don't aggravate the issue. Always wear stable, supportive shoes—ideally with your orthotic inserts—to give your feet a solid foundation.
Low-impact activities are usually your best friend. Consider these excellent choices:
- Cycling: Gives you a great cardio workout with minimal stress on your arches.
- Swimming: A fantastic full-body workout with zero impact on your feet.
- Yoga or Pilates: Can help improve flexibility, balance, and core strength, all of which support your entire body.
The most important rule? Listen to your body. If you feel any new or worsening pain, that's your cue to stop, rest, and rethink your approach, maybe with some guidance from a professional.
Does Walking Barefoot Help or Hurt Fallen Arches?
This is a great question, and the answer really comes down to one thing: the surface you're walking on.
Walking barefoot on soft, uneven ground like sand or a grassy lawn can actually be helpful. It makes the small, deep muscles in your feet work harder, which can gradually strengthen them over time.
On the other hand, spending a lot of time barefoot on hard, flat surfaces like tile, wood, or concrete is a completely different story. With no support, you're just adding more strain to your arches, which can make your symptoms worse. For everyday life indoors on hard floors, supportive shoes or slippers are almost always the better choice.
If you're tired of foot pain dictating your day, it's time to give your feet the support they've been missing. Samurai Insoles are biomechanically designed in an American orthotic lab specifically to fight overpronation and ease the pain from fallen arches. Stop putting up with discomfort and discover which of our targeted insoles is right for your feet. Experience the relief for yourself at SamuraiInsoles.com.



