The Morning Heel Pain Reality Check
That first excruciating step out of bed isn't just a random ache; it's a shared experience for millions. If your morning routine begins with a sharp, stabbing pain in your heel, you’re not alone. Understanding what causes plantar fasciitis starts with acknowledging just how common this condition is. It isn't simply bad luck—it's a widespread problem with clear, identifiable patterns.

Who Is Really at Risk?
The statistics paint a clear picture. Plantar fasciitis affects approximately 10% of the global population at some point in their lives, making it one of the most common causes of foot pain. In the United States, about 2 million people seek treatment for it every year. The condition is most common in adults between the ages of 40 and 60, and this is no coincidence. You can discover more about these worldwide statistics at mentonegeneralpractice.com.au.
When we look at patient data and talk to podiatrists, it becomes obvious that certain factors like age, job, and lifestyle can put you on a direct path to heel pain. Many people live with this discomfort for months before they even realize their morning agony has a name. Pinpointing the pain's location is often the first step toward a proper diagnosis. You can learn more about where plantar fasciitis pain is located in our guide.
The Economic Reality of Heel Pain
Beyond the physical pain, there is a real financial cost to consider. Getting to the root causes is important not just for relief but also for avoiding the expensive and frustrating cycle of treatments that many people get stuck in. By identifying your personal risk factors, you can take proactive steps to protect both your feet and your wallet. This guide will walk you through the forces at play, from the big-picture statistics to the specific biomechanics and lifestyle habits behind the pain.
Inside Your Foot's Engineering Marvel
Think of your foot as a high-performance suspension bridge. Every single day, it carries the entire weight of your body, absorbing incredible force with each step. The secret to this amazing feat of natural engineering is the plantar fascia, a thick, strong band of tissue running from your heel bone to the base of your toes. It works like a taut bowstring, maintaining your foot's essential arch and providing vital shock absorption.

The Fascia's Unique Design
Your plantar fascia is engineered for toughness, able to withstand forces equal to 2-3 times your body weight when you walk or run. However, this impressive strength has a major drawback. Unlike muscles, which are rich with blood vessels, the plantar fascia has a very limited blood supply. This quality makes it remarkably durable but also frustratingly slow to heal when injured.
This dual nature is key to understanding what causes plantar fasciitis. A primary cause of the condition is repetitive microtrauma to this crucial tissue. Over time, these tiny tears build up, causing irritation and inflammation that your body struggles to fix because of the poor blood flow. You can discover more insights about foot biomechanics on kurufootwear.com. This slow healing is why the pain can become persistent and disruptive.
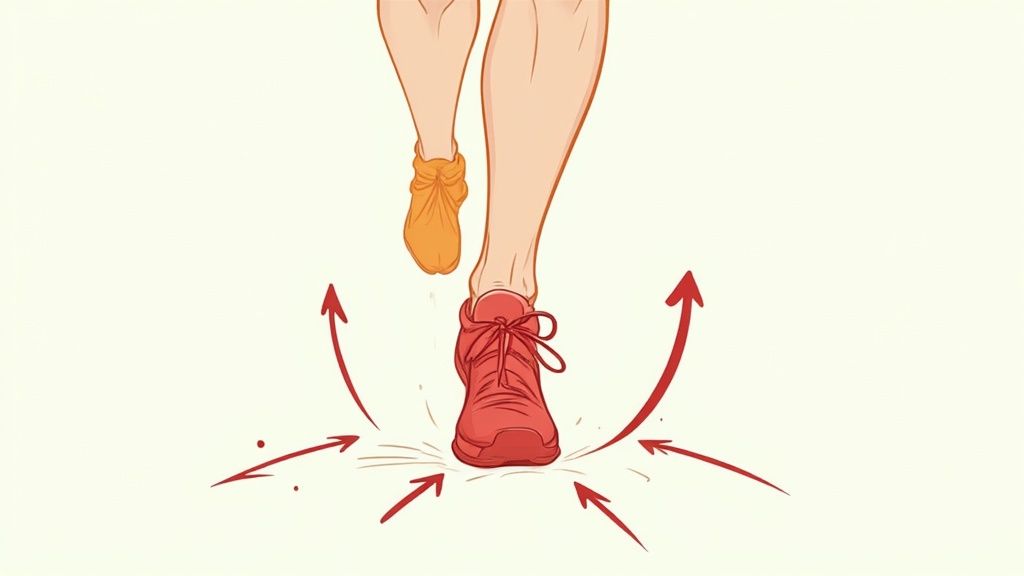
A Symphony of Movement and Stress
The plantar fascia does not operate alone; it's a key player in an interconnected system. It works closely with your heel bone (the calcaneus), your arch, and the joints of your toes to produce a smooth, efficient walking and running motion. This is known as the windlass mechanism. When you push off the ground, your toes bend upward, tightening the fascia just like winding a winch. This action lifts the arch, makes the foot rigid, and creates a strong lever for pushing forward.
However, this brilliant design also has points of weakness. The areas where the fascia connects to the heel bone and stretches across the arch are put under immense tension. When factors like unsupportive footwear, abrupt increases in activity, or certain foot shapes throw this delicate balance off, the tissue becomes overloaded. This leads to the microscopic damage that ultimately results in plantar fasciitis.
When Your Body's Movement System Breaks Down
Your body doesn't operate like a collection of separate parts; it's an interconnected system where everything works together. When one component isn't pulling its weight, it can set off a domino effect that travels all the way down to your foot. This breakdown in your body's mechanics, known as biomechanical dysfunction, is a key reason why plantar fasciitis develops. Issues that seem unrelated, like tight calf muscles or weak hips, can dramatically increase the strain on your plantar fascia.
The Kinetic Chain Reaction
Picture your body's movement system as a chain. If one link is weak or stiff, the other links must overcompensate to get the job done. This compensation often leads to overload and stress in another area. For example, tight calf muscles can limit your ankle's range of motion, which alters how your foot rolls with each step. This subtle change forces the plantar fascia to absorb much more shock than it's built to handle.
This chain reaction isn't limited to the ankle. A foot that's out of alignment can affect your knees, which in turn changes how your hip muscles have to work when you walk or run. Over time, these small adjustments and compensations build up, creating the perfect conditions for your plantar fascia to become overworked and painful.
Common Biomechanical Triggers
Several well-known structural and functional problems put extra stress on the plantar fascia. These issues interfere with the foot's natural ability to absorb impact and spread weight evenly.
To better understand these factors, the table below breaks down common biomechanical issues, explaining how each one contributes to plantar fasciitis.
| Risk Factor | How It Affects Plantar Fascia | Prevalence | Prevention Strategy |
|---|---|---|---|
| Flat Feet (Pes Planus) | Causes the foot arch to collapse and roll inward (overpronation), which overstretches and pulls on the plantar fascia with every step. | Affects 20-30% of the general population. | Wear supportive shoes with good arch support, use orthotic inserts, and perform foot-strengthening exercises. |
| High Arches (Pes Cavus) | Creates a rigid foot that is poor at absorbing shock. Impact forces are concentrated on the heel and ball of the foot, overloading the fascia. | Less common, affecting about 8-15% of the population. | Choose cushioned footwear to improve shock absorption, and perform stretches for the plantar fascia and calf muscles. |
| Tight Calf Muscles | Limits the ankle's ability to flex (dorsiflexion), forcing the foot to pronate more to compensate. This increases tension on the fascia. | Very common, especially in active individuals and those who sit for long periods. | Regular calf stretching, foam rolling, and ensuring proper warm-ups before exercise. |
| Weak Hip & Core Muscles | Leads to poor control of the leg during movement, often causing the knee to collapse inward. This alters gait mechanics and increases stress on the foot. | Common in both sedentary and active populations, often overlooked. | Incorporate hip and core strengthening exercises like bridges, clamshells, and planks into your routine. |
This table highlights how different body mechanics can lead to the same painful outcome. What works as a preventive measure for one person might be different for another, depending on their unique biomechanics.
Ultimately, these mechanical quirks are why some people can run for miles without a problem, while others get heel pain just from their daily routine. As we get older, our tissues also lose some of their natural flexibility. This makes these minor mechanical faults much more likely to turn into significant sources of pain.
The Hidden Lifestyle Saboteurs
Sometimes, the culprit behind plantar fasciitis isn't a dramatic injury but the quiet, steady strain of your everyday life. The very lifestyle choices you make—even the healthy ones—can secretly push your plantar fascia past its breaking point. That standing desk you got for better posture, your adventurous weekend hikes, or even hitting your daily 10,000 steps can each contribute to overloading this vital tissue.

Occupational Overload
Take a moment to think about your job. Are you on your feet for most of the day? For professionals like teachers, nurses, and retail workers, standing for hours on hard floors is a major risk factor. This constant pressure robs the plantar fascia of the downtime it needs to repair itself, leading to the painful micro-tears that define the condition. Each day layers on a bit more stress, leaving the tissue increasingly vulnerable over time.
The Weekend Warrior Effect
At the other end of the spectrum is the classic "weekend warrior." This pattern involves sitting at a desk all week, only to launch into high-intensity activities on a Saturday morning. Your body's ability to adapt simply can't keep up with your enthusiasm. Tissues that have grown accustomed to a sedentary week are suddenly forced to perform at peak level. This sharp increase in activity is a textbook formula for straining a plantar fascia that wasn't prepared for the demand.
This imbalance creates a frustrating cycle of damage and incomplete healing, which slowly wears down your foot's natural resilience. Simply recognizing these subtle lifestyle patterns is the first step toward breaking the cycle. If you're already feeling the twinges of pain, learning how to treat plantar fasciitis with effective methods can offer relief and help you sidestep future problems. The goal is to find a healthy balance between your activity levels and your body's true capacity for recovery.
Your Shoes Are Speaking - Are You Listening?
Every step you take is a conversation between your feet and the ground, with your shoes acting as the interpreter. When that interpretation is poor, your plantar fascia often bears the brunt of the miscommunication. Footwear is a major factor in what causes plantar fasciitis, and the culprits might be hiding in plain sight in your closet. For instance, those beloved old sneakers may feel perfectly broken-in, but they are more likely broken-down. Over time, the supportive materials inside a shoe compress and wear out, losing their ability to absorb impact and leaving your plantar fascia to take on the stress alone.
The Hidden Dangers in Your Closet
Some of the most popular shoe styles are notorious for causing foot problems. Take flip-flops, for example. Their complete lack of structure means your toes must constantly grip the sole just to keep them on your feet. This seemingly minor action creates a ripple effect of tension that travels directly to your plantar fascia, adding strain with every step.
High heels create an entirely different set of issues. By elevating your heel, they shorten your calf muscles and shift your body's weight forward onto the ball of your foot. This unnatural alignment dramatically increases the load on your plantar fascia. This isn't just a temporary problem; prolonged wear can lead to lasting changes in your walking pattern, stressing your feet even when you're barefoot.
Cushioning vs. Support: Finding the Right Balance
Even shoes designed for "comfort" can be deceptive. Ultra-cushioned shoes might feel like walking on clouds at first, but this can come at a cost. Excessive padding can prevent the small, intrinsic muscles in your feet from doing their job, leading to weakness over time. A weaker foot structure is less stable and more prone to the micro-tears that define plantar fasciitis.
The goal is to find shoes that support your foot's natural mechanics, not work against them. A good shoe should feel like a partner to your foot, not a crutch. To protect your feet, look for these key features in your footwear:
- Adequate Arch Support: This helps maintain the natural shape of your foot and prevents the plantar fascia from overstretching.
- Sufficient Cushioning: Good cushioning, especially in the heel, absorbs the shock that would otherwise travel straight to the fascia.
- A Sturdy Heel Counter: The firm part at the back of the shoe, a sturdy heel counter provides stability and controls excessive side-to-side foot motion.
To better understand how your shoe choices stack up, let's look at a direct comparison of common footwear types and their associated risks.
Table: Footwear Impact on Plantar Fasciitis Risk
Analysis of how different shoe types affect plantar fascia stress and injury risk
| Shoe Type | Risk Level | Main Problems | Recommended Use |
|---|---|---|---|
| High Heels | High | Unnatural foot angle, shortened calf muscles, immense pressure on the plantar fascia. | Special occasions only; limit wear time significantly. |
| Flip-Flops | High | No arch support, no heel cushion, forces toes to grip, causing continuous fascia strain. | Poolside or beach use; not for walking long distances. |
| Worn-Out Sneakers | High | Compressed cushioning and broken-down support structures offer no shock absorption. | Discard or relegate to non-walking activities like gardening. |
| Minimalist/Barefoot Shoes | Medium | Can be beneficial for strengthening feet but offers little protection on hard surfaces if not properly conditioned. | Short-term use on soft surfaces; requires gradual adaptation. |
| Flat Dress Shoes | Medium | Often lack sufficient arch support and cushioning, leading to fascia strain over a full workday. | Look for models with built-in support or use orthotic inserts. |
| Supportive Athletic Shoes | Low | Designed with proper arch support, heel cushioning, and stability to protect the foot during activity. | Daily wear, exercise, and for periods of prolonged standing or walking. |
As the table shows, shoes with poor support and either too little or too much cushioning pose the greatest risk. Making informed footwear choices is a critical step in preventing the chronic stress that leads to plantar fasciitis.
The Perfect Storm: Weight, Activity, And Time
Certain factors can combine to create the ideal conditions for plantar fasciitis to develop. These elements—your body weight, activity level, and the simple passage of time—are closely connected. Each one can amplify the effects of the others, and understanding how they work together is crucial to knowing what causes plantar fasciitis.
The Math of Body Weight and Foot Stress
Think of your plantar fascia as a support cable designed to handle significant force, but even the strongest cable has its limits. Every extra pound of body weight you carry translates to roughly four additional pounds of force on your feet and fascia with every step you take. This constant, magnified pressure can slowly lead to the tiny tears that cause chronic heel pain, particularly for individuals who are overweight.
The Activity and Aging Paradox
Next, let's look at the tricky relationship between how active you are and how old you are. A sedentary lifestyle can weaken the supportive muscles in your feet, leaving your plantar fascia more vulnerable to strain. On the other hand, a sudden jump in activity—like deciding to train for a 5K over a weekend—can easily overwhelm tissues that have grown less flexible over the years.
As we get older, our plantar fascia naturally loses some of its elasticity and its ability to repair itself quickly. For women, hormonal changes can also affect tissue quality. This creates a difficult scenario where multiple factors work against you:
- Inactivity weakens the foot's natural support structure.
- A sudden increase in activity overloads the unprepared fascia.
- Age reduces the tissue's ability to bounce back from the stress.
When these three factors—weight, a change in activity, and age—come together, the total stress can become more than the plantar fascia can bear, leading to persistent and often frustrating pain.
When Your Body Betrays Your Feet
Sometimes, that stubborn heel pain isn't just about your feet. It can be a warning sign from your body, pointing to other health issues creating trouble downstream. In these cases, your plantar fascia acts like a canary in a coal mine. Understanding what causes plantar fasciitis means looking beyond just your feet, as certain medical conditions can turn a minor foot strain into a chronic, debilitating problem.
Systemic Health and Heel Pain
Think of your body's healing process as a bustling factory. If key departments, like blood circulation or inflammation control, aren't running smoothly, the whole production line suffers. For example, conditions like diabetes can reduce blood flow to your hands and feet. This means your feet don't get enough of the vital nutrients and oxygen needed to repair tissue, making it much harder for those small micro-tears in the fascia to heal.
Similarly, some autoimmune conditions can cause widespread inflammation throughout the body. This makes your connective tissues, including the plantar fascia, more prone to irritation and injury. Even certain medications, like specific types of antibiotics, have been linked to weaker tendons and ligaments, creating an unexpected risk factor for foot pain.
When to Look for a Deeper Cause
If your heel pain keeps coming back no matter how diligently you follow treatment plans, it might be time to look for a broader cause. Conditions like thyroid disorders can affect tissue health, while chronic stress and even sleep apnea can disrupt your body's natural repair cycles. A full medical check-up can sometimes uncover these surprising underlying issues.
Here are a few scenarios where your heel pain might signal a larger problem:
- Recurring Pain: The pain returns again and again, despite consistent stretching, proper footwear, and rest.
- Bilateral Symptoms: You have pain in both feet at the same time, which could suggest a systemic issue rather than a mechanical one.
- Other Unexplained Symptoms: You're also experiencing joint pain in other parts of your body, constant fatigue, or other unusual symptoms.
In these situations, your heel pain might be a symptom, not the root problem. Getting to the bottom of the underlying medical condition could be the key to finally finding lasting relief.
Your Personal Plantar Fasciitis Prevention Plan
Understanding what causes plantar fasciitis helps you move from just reacting to pain to actively preventing it. This isn't about a generic checklist but about building a plan that fits your unique body and daily life. By taking a moment to review your own habits and physical traits, you can spot your personal risk factors before they cause a serious injury.
Conducting Your Risk Self-Assessment
Begin by looking at your personal profile. Consider the key areas that contribute to heel pain:
- Biomechanics: Do you have flat feet or high arches? Has a professional ever mentioned that you overpronate (your foot rolls inward too much)? Are your calf muscles always tight, no matter what you do?
- Lifestyle & Occupation: Does your job keep you standing or walking on hard floors for more than four hours a day? Are you a "weekend warrior," packing intense exercise into just one or two days?
- Footwear: Take an honest look at the shoes you wear most often. Are they worn out, missing arch support, or completely flat like many flip-flops or old dress shoes?
- Weight & Age: Are you carrying extra weight that puts more pressure on your feet? Are you over the age of 40? Our body's tissues naturally lose some flexibility as we get older.
Answering these questions gives you a clear picture of where your biggest risks lie.
Recognizing Early Warning Signs
Long before sharp pain appears, your body often sends out subtle signals. Learning to recognize these early warnings is key to prevention. Pay attention to:
- A slight stiffness or a dull ache in your heel when you take your first steps in the morning.
- A feeling of soreness in your arch after a long day on your feet.
- Your feet feeling tired more quickly after activities that used to feel easy.
These aren't just minor annoyances; they are your plantar fascia's way of telling you it's under too much strain. By addressing these early signs with targeted stretching, better footwear, and supportive insoles, you can often stop the condition from getting worse. You can read our guide on how plantar fasciitis insoles fix heel pain to see how simple support can make a huge difference.
Don't wait for the pain to become unbearable before you take action. Samurai Insoles are designed to help correct the biomechanical imbalances that cause strain, giving you a simple but effective tool for your prevention plan. Find the right insoles for your feet today.



