That First Step Of The Day (And Why It Hurts So Much)
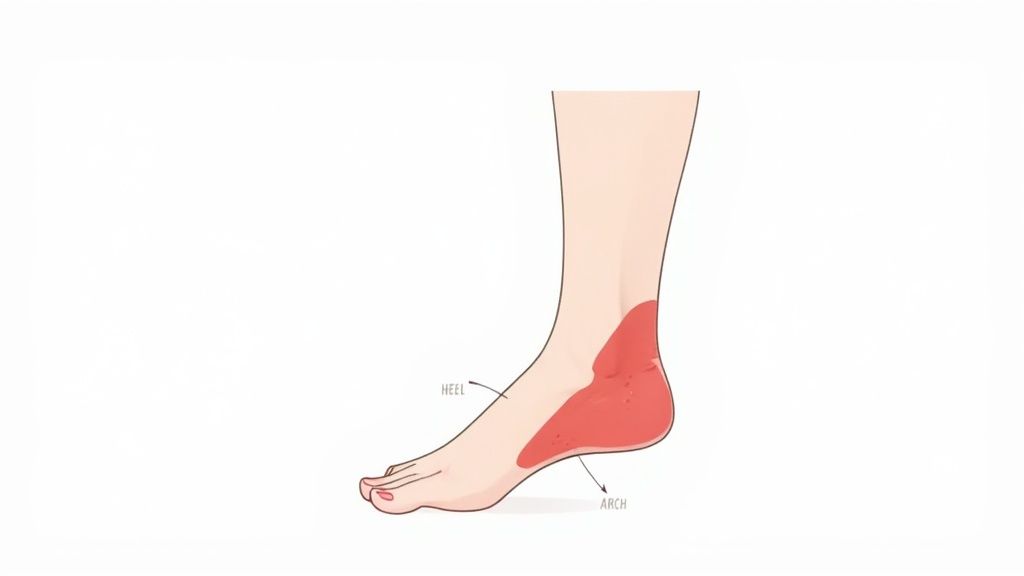
If you dread the sound of your morning alarm, not because of the day ahead, but because of the first step you’ll take, you understand the core experience of plantar fasciitis. That sharp, stabbing pain in your heel when you get out of bed is the condition’s most notorious symptom. It’s often described as stepping on a nail or a piece of glass—a jarring sensation that can make you gasp.
This intense morning pain isn't random; it’s a direct result of what happens while you sleep. Overnight, your foot is typically in a relaxed, pointed position, a state known as plantar flexion. This allows the inflamed and irritated plantar fascia—the thick band of tissue connecting your heel to your toes—to shorten and tighten. Picture it like a rubber band that has been left to contract for hours.
The Science Behind The Shock
When you finally place your foot on the floor and put weight on it, you are abruptly stretching that cold, contracted tissue. This sudden strain on the tiny tears within the fascia is what creates that acute, sharp pain. This is why those first several steps are often the most painful part of the day.
As you walk around, the fascia begins to warm up and stretch out, which is why the pain often eases into a dull ache. However, the relief is usually temporary. The pain cycle repeats after any long period of inactivity, like standing up after sitting at a desk for an hour. This distinct pattern of pain-after-rest is a key indicator of plantar fasciitis. Understanding this cycle is the first step toward managing the condition effectively.
The Language Of Heel Pain (How People Really Describe It)
 While we’ve covered the mechanics of that dreaded "first-step" pain, the sensations themselves can be surprisingly diverse. When patients are asked what plantar fasciitis feels like, their descriptions are often vivid and consistent. These feelings aren't random; they are your body's way of translating the specific tissue damage in your foot into a language your brain can understand.
While we’ve covered the mechanics of that dreaded "first-step" pain, the sensations themselves can be surprisingly diverse. When patients are asked what plantar fasciitis feels like, their descriptions are often vivid and consistent. These feelings aren't random; they are your body's way of translating the specific tissue damage in your foot into a language your brain can understand.
This "message" from your foot usually starts with a classic stabbing or piercing feeling, especially after periods of rest. This particular sensation happens because the plantar fascia has developed microtears and inflammation from ongoing stress, causing it to tighten up. When you suddenly put weight on it, that rigid, damaged tissue protests by sending sharp pain signals. You can explore the science behind this symptom in more detail through medical literature on foot pain.
However, the "language" of your pain can change throughout the day, giving you important clues about how your foot is doing.
Decoding Different Pain Sensations
The personality of your pain can shift from sharp and stabbing to other distinct feelings. Learning to interpret these variations helps you understand the different phases of irritation or healing. Common descriptions include:
- Burning Pain: This hot, searing feeling often runs along the arch or is concentrated at the heel. It typically points to active inflammation and irritated nerves. Think of it as the tissue sending an urgent "SOS" signal.
- Dull Ache or Throbbing: This sensation usually appears after you've been on your feet for a while. Once the initial sharpness subsides, a deep, persistent ache can settle in. This is the "aftermath" pain, reflecting the total stress placed on the already-injured fascia.
- Tenderness to Touch: The spot just in front of your heel bone—where the fascia connects—might feel bruised or extremely tender when you press on it. This localized sensitivity pinpoints the epicenter of the injury.
Recognizing these different types of pain is key. A sudden return of sharp, burning pain could mean you've pushed yourself too hard, whereas a gradual shift to a dull ache might suggest you're on the path to recovery.
When Heel Pain Travels (The Surprising Ripple Effects)

While your heel might feel like ground zero for the pain, it rarely stays there. Your body is incredibly smart and will do whatever it can to avoid pain. When your foot hurts, you subconsciously change how you walk to protect the sore spot. This adjustment creates a chain reaction of strain that can travel far beyond your foot.
These changes are known as compensatory patterns, and they are your body's way of finding the path of least resistance. You might start landing more on the outside of your foot or begin favoring your "good" leg. Think of it like driving a car with a slightly deflated tire—it might not seem like a big deal at first, but eventually, other parts start to wear down from the imbalance.
The Unseen Domino Effect
This unconscious compensation can cause a variety of secondary aches and pains that might seem completely unrelated to your foot. Recognizing these ripple effects is crucial for understanding the full picture of what plantar fasciitis feels like. Some of the most common issues include:
- Calf Tightness: Your calf muscles often work overtime to stabilize your foot and ankle, leading to tightness and soreness as you alter your walking motion.
- Arch Soreness: While the pain starts at the heel, it can spread through the entire arch as the whole plantar fascia ligament remains under constant stress.
- Opposite Leg Discomfort: Your other leg has to pick up the slack, which can lead to fatigue and new pain in the hip, knee, or even the other foot.
- Lower Back Pain: An uneven walking pattern can subtly tilt your pelvis. Over time, this imbalance puts new and unfamiliar strain on your lower back muscles.
2. Pain Triggers That Catch You Off Guard
Beyond the well-known morning pain, plantar fasciitis has a knack for showing up uninvited throughout your day. That sharp, stabbing sensation you feel when getting up from your office chair isn't random—it's a classic sign of the condition. Just like when you sleep, sitting for a long time allows the plantar fascia to shorten and tighten. When you finally stand, the sudden weight forces it to stretch unexpectedly, causing that familiar jolt of pain.
Think of it like a cold rubber band. If you let it sit, it becomes stiff. Try to stretch it quickly, and it's likely to snap or resist painfully. This is what happens to your plantar fascia after periods of rest, helping to explain what plantar fasciitis feels like in everyday scenarios.
Common Scenarios That Amplify Heel Pain
Certain activities and environments are known troublemakers for plantar fasciitis. Knowing what they are allows you to anticipate the pain and take steps to prevent a flare-up.
Here are some of the most common triggers:
- Long Periods of Standing: Jobs in fields like nursing, retail, or food service that keep you on your feet for hours put constant, grinding pressure on your plantar fascia. The tissue never gets a chance to rest, which can lead to a deep, throbbing ache that gets worse as the day goes on.
- Hard, Unforgiving Surfaces: Walking or standing on concrete, tile, or hardwood floors without proper footwear is like making your feet walk a tightrope without a safety net. These surfaces offer zero shock absorption, forcing your plantar fascia to absorb the full impact of every step.
- A Sudden Increase in Activity: Maybe you felt great and decided to go for a 5-mile run after weeks of inactivity, or you spent a full day walking around a new city on vacation. This kind of "too much, too soon" activity can easily overwhelm the fascia, causing tiny tears and triggering inflammation.
To help you connect these triggers to your own experience, the table below breaks down how different daily activities can impact your pain levels and what you can do in the moment for relief.
| Activity/Situation | Typical Pain Level | Why It Hurts | Quick Relief Tips |
|---|---|---|---|
| Getting Out of Bed | High | The plantar fascia has tightened and shortened overnight. The first steps of the day force a sudden, painful stretch. | Before standing, gently flex your foot up and down 10-15 times. Massage the arch of your foot with your thumbs for a minute. |
| Sitting for 1+ Hour | Moderate to High | Similar to sleeping, prolonged sitting allows the fascia to stiffen. The pain strikes upon standing. | Roll a tennis or lacrosse ball under your foot while seated. Stand up slowly, putting weight on your foot gradually. |
| Standing All Day | Moderate (Ache) | Continuous strain and pressure on the fascia lead to cumulative fatigue and inflammation, often felt as a dull, throbbing pain. | Wear supportive shoes with good arch support. Take short sitting breaks. Do gentle calf stretches throughout the day. |
| Walking on Concrete | Moderate to High | Hard surfaces provide no cushioning, so the full force of each step is absorbed by your foot, jarring the inflamed fascia. | Wear cushioned, supportive footwear. Avoid going barefoot on hard floors. Use orthotic inserts for extra shock absorption. |
| Intense Exercise | High (Often After) | High-impact activities like running or jumping cause micro-tears in the fascia. The pain may be worse after you cool down. | Warm up properly with dynamic stretches. Ice your heel for 15-20 minutes after the activity. Ensure your athletic shoes are not worn out. |
Understanding these patterns is the first step toward taking back control. When you can anticipate what will cause a flare-up, you can move from just reacting to the pain to actively managing your foot health. This proactive approach is a cornerstone of a successful recovery.
The Life You Didn't Plan (How Chronic Heel Pain Changes Everything)
Plantar fasciitis does more than just cause foot pain; it quietly begins to reshape your entire life. You start making decisions not based on what you want to do, but on what your heel can handle. A simple walk in the park, a spontaneous shopping trip, or a standing-room-only concert becomes a complex mental calculation of how much pain you'll be in later. This constant negotiation is draining and often goes unnoticed by others.
The frustration is a major part of the experience. It can feel isolating to explain to friends for the third time why you can’t join their weekend hike. You might find yourself checking a mental "foot forecast" each morning, anxious about whether it will be a good pain day or a bad one. This emotional burden, all stemming from what seems like a simple foot problem, is a real and frequently overlooked part of what plantar fasciitis feels like.
The Hidden Costs Of Chronic Pain
The consequences of chronic heel pain spread into almost every part of daily life, creating challenges that are more than just physical. These hidden impacts show why finding real relief is about more than just your feet—it's about getting your quality of life back.
- Emotional & Social Toll: The cycle of pain and physical limits can take a toll on your mood and relationships. Missing out on activities you once loved can lead to irritability or sadness.
- Work Performance: For many, especially those in jobs that require standing or walking, the pain directly affects their ability to perform. This can impact both focus and productivity.
- Financial Burden: The costs of managing the pain also accumulate. Studies reveal that about 93% of adults with plantar fasciitis spend money on treatment every month, and nearly 28% spend over $250 monthly. You can explore more about these expenses in this detailed breakdown of plantar fasciitis statistics.
Recognizing these wider effects is the first step toward taking control. It underscores the importance of finding a solution that offers dependable relief. To begin your recovery journey, you might find this guide on how to treat plantar fasciitis for real relief that works helpful.
Is It Really Plantar Fasciitis? (Sorting Through Similar Heel Pain)
 Just because your heel hurts doesn't automatically mean you have plantar fasciitis. Several other conditions can cause similar symptoms, making a proper diagnosis the most important step for effective treatment. Think of your heel pain as a distress signal; different conditions send that signal from slightly different locations and at different times. Pinpointing the true source is key to finding relief.
Just because your heel hurts doesn't automatically mean you have plantar fasciitis. Several other conditions can cause similar symptoms, making a proper diagnosis the most important step for effective treatment. Think of your heel pain as a distress signal; different conditions send that signal from slightly different locations and at different times. Pinpointing the true source is key to finding relief.
A common point of confusion is the heel spur, which is a bony growth on the heel bone. While they sound painful, spurs themselves are often painless. They can develop in response to the same long-term strain that causes plantar fasciitis, making them more of a side effect than the root cause of the pain. It's usually the inflamed tissue, not the bone, that hurts.
Distinguishing The Imposters
So, what does plantar fasciitis feel like compared to other conditions? The location and timing of your pain offer the biggest clues. For example, Achilles tendinitis pain is typically felt higher up on the back of the heel or ankle, not on the sole of your foot. A stress fracture, on the other hand, usually creates a more constant, sharp pain in one spot that gets worse with activity and doesn't improve much with rest.
To help you tell these conditions apart, the table below outlines the key differences in how and when the pain appears.
| Condition | Primary Pain Location | Worst Pain Timing | Distinguishing Characteristics |
|---|---|---|---|
| Plantar Fasciitis | Bottom of the heel, sometimes into the arch | First steps in the morning or after rest | Stabbing pain that often improves with light activity but worsens after long periods of standing. |
| Heel Spur | Bottom of the heel (often co-exists with Plantar Fasciitis) | Can be constant or intermittent | Often causes no pain on its own; pain is usually from associated tissue inflammation. Visible on an X-ray. |
| Achilles Tendinitis | Back of the heel or lower calf | During and after activity, especially running or jumping | Pain and stiffness along the Achilles tendon; swelling may be present. |
| Tarsal Tunnel Syndrome | Inside of the ankle and bottom of the foot | Often worse at night or with prolonged standing/activity | Burning, tingling, or numbness, similar to Carpal Tunnel Syndrome but in the foot. |
| Stress Fracture | A specific, localized point on the heel bone | Worsens progressively with activity, constant deep ache | Pain that doesn't ease with rest; tenderness directly over the fracture site. |
This table shows why a one-size-fits-all approach to heel pain doesn't work. Each condition has a unique signature that points toward a different treatment path.
Getting the diagnosis wrong can lead you down a frustrating path of ineffective treatments. Understanding these subtle but important differences is crucial. If you want to learn more about what directly triggers this condition, you can read our article on what causes plantar fasciitis and the key factors you should know. A clear diagnosis from a healthcare professional ensures you target the actual problem, saving you time, frustration, and further pain.
You're In Good (But Sore) Company
 If that sharp, stabbing heel pain has you thinking you're alone in your misery, take a little comfort in knowing you've just joined a very large club. From nurses logging miles on hospital floors to runners pushing their limits, plantar fasciitis is an incredibly common foot problem. It’s not a personal failure, but a widespread issue that comes from the daily demands we put on our feet.
If that sharp, stabbing heel pain has you thinking you're alone in your misery, take a little comfort in knowing you've just joined a very large club. From nurses logging miles on hospital floors to runners pushing their limits, plantar fasciitis is an incredibly common foot problem. It’s not a personal failure, but a widespread issue that comes from the daily demands we put on our feet.
Who Gets Plantar Fasciitis?
This condition doesn't discriminate, affecting people from all walks of life. In fact, research shows it's one of the most frequent causes of heel pain, impacting roughly 1 in 10 people at some point in their lives. While it is most common in adults between the ages of 40 and 60, it also regularly appears in younger, more active individuals. You can learn more about its prevalence by exploring some statistics on plantar fasciitis worldwide.
Several factors can increase your chances of developing it:
- Jobs that keep you standing or walking for long hours.
- High-impact activities like running, dancing, or aerobics.
- Foot structure, including having flat feet or unusually high arches.
Realizing that millions of others have experienced the same frustrating pain can change your perspective. It’s a confirmation that this is a manageable condition, not a permanent sentence. With the right approach and a bit of patience, you can get back to living without that morning dread.
Finding the right support often starts from the ground up. Discover how Samurai Insoles can provide the relief you need and take the first step toward a more comfortable future.



