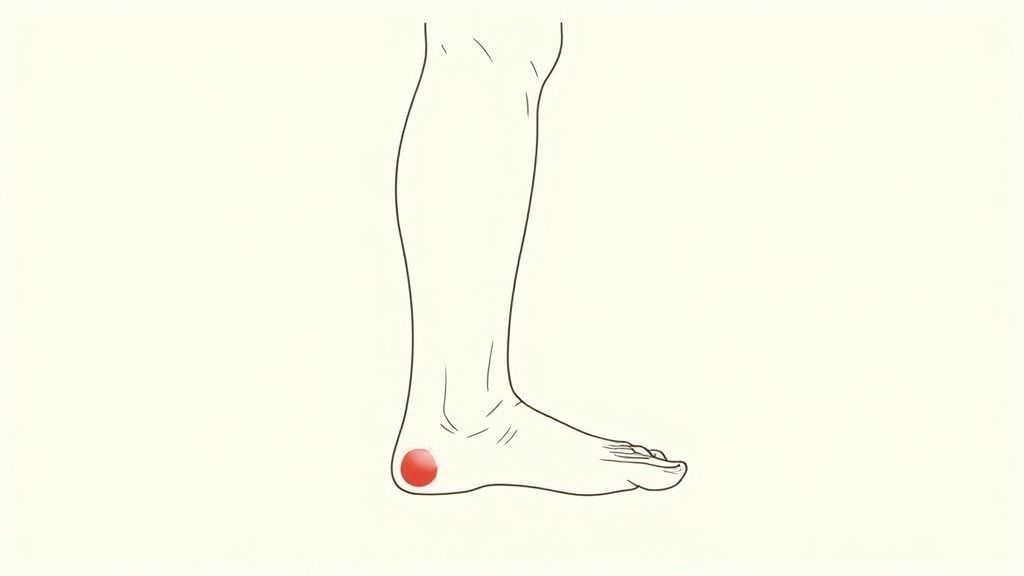
Yes, plantar fasciitis can absolutely cause ankle pain. It might seem strange since the injury is in your heel, but it's a classic case of one problem leading to another. The ankle pain isn't just a coincidence; it's a direct result of your body trying to shield you from that sharp, stabbing sensation in your foot.
Connecting Heel Pain To Ankle Discomfort
When that first step out of bed feels like walking on a sharp rock, your instincts take over. You immediately change the way you walk to avoid the pain. This is a survival mechanism, but it comes at a cost.

Why Your Body Overcompensates
This subtle shift in how you walk is called gait compensation. It’s your body's attempt to offload pressure from your painful heel. You might start walking on the outside of your foot, shortening your stride, or even limping.
Think of it like trying to drive a car with a flat tire. To avoid damaging the rim, you slow down and steer awkwardly, putting immense strain on the other three tires and the car’s alignment. Over time, that compensation creates new problems.
Your body does the same thing. By changing your natural walking motion, you’re forcing the muscles, tendons, and ligaments around your ankle to do jobs they weren't designed for. This abnormal stress creates a chain reaction, leading to overuse, inflammation, and a brand-new ache in your ankle.
The ankle pain isn't the root issue. It’s a secondary symptom caused by your body creating a workaround that, while temporarily protecting the heel, ends up overloading the ankle joint.
This is an incredibly common scenario. Plantar fasciitis is the leading cause of heel pain, affecting roughly 10% of people at some point in their lives. Pre-existing issues like poor ankle flexibility can make things even worse, as they already alter your foot’s mechanics and set the stage for this kind of compensatory stress. You can find more details in research exploring plantar fasciitis risk factors and their impact on how we walk.
To make it even clearer, here’s a quick breakdown of that chain reaction from heel pain to ankle trouble.
How Heel Pain Leads to Ankle Pain: A Simple Breakdown
| The Cause | The Body's Reaction | The Result |
|---|---|---|
| Sharp, localized pain in the heel from plantar fasciitis. | You change your natural walking pattern (your gait) to avoid the pain. | The muscles, tendons, and ligaments around your ankle become overworked, strained, and inflamed. |
This table shows how a simple protective instinct can snowball, turning one source of pain into two. Addressing the root cause—the plantar fasciitis—is the only way to break the cycle and find lasting relief for both your heel and your ankle.
What Is Plantar Fasciitis Really Doing to Your Foot?
To understand how plantar fasciitis can mess with your ankle, we first have to get to the root of the problem in your foot. Picture the plantar fascia: it’s like a tough, springy ligament that runs along the bottom of your foot, connecting your heel to the base of your toes and creating your arch.
When this ligament gets overworked, tiny tears develop, and it becomes inflamed. That inflammation is what delivers that classic, sharp, stabbing pain in your heel—especially with those first dreaded steps out of bed.
The Common Culprits Behind the Pain
So, what puts all that stress on your plantar fascia in the first place? It’s usually not one single event but rather a build-up of strain from your daily habits or how your foot is built.
The most frequent triggers I see are:
- Long Hours on Your Feet: If your job keeps you standing or walking all day, you're putting constant, repetitive pressure on your arches.
- Unsupportive Footwear: Flimsy shoes with no arch support or heel cushioning are a major problem. They don't absorb impact, forcing your plantar fascia to take the full brunt of every step.
- Your Foot Shape: Having either very flat feet or unusually high arches can change how your weight is distributed, putting extra strain on that ligament.
- Tight Calf Muscles: This is a big one. When your calf muscles are tight, they pull on your heel bone, which in turn yanks on the attached plantar fascia.
This is more than just a little foot pain. The stabbing sensation in your heel is your body's alarm bell, signaling damage and inflammation. When you ignore it, you don't just put up with the heel pain; you start walking differently to avoid it. That’s when the ankle trouble begins.
Getting this connection is key. By focusing on how to treat your plantar fasciitis, you start fixing the source of the problem. That not only helps your heel but also stops the chain reaction that's hurting your ankle. You can learn more in our detailed guide on how to treat a plantar fasciitis. It's the only way to truly break the cycle of pain.
How Your Limp Puts Your Ankle on the Line
When that sharp, stabbing pain hits your heel with every step, you naturally start walking differently to avoid it. We all do it. This reaction is your body's attempt to protect itself, and it has a clinical name: an antalgic gait. It’s simply a fancy way of saying you’re limping to minimize pain.
This new way of walking is the crucial link between your plantar fasciitis and that new, nagging ache in your ankle. Instead of the normal, fluid heel-to-toe roll, you might find yourself walking on your toes, favoring the ball of your foot, or rolling onto the outer edge. It feels like a small change, but for your body's mechanics, it's a huge disruption.
Why Limping Creates a New Problem
Think of your ankle as a finely tuned hinge, built with a specific set of bones, tendons, and ligaments designed for a particular range of motion. When you start walking funny to spare your sore heel, you throw that entire system out of whack.
If you roll your foot outward, for instance, you're putting a ton of unexpected stress on the tendons running along the outside of your ankle. Roll it inward, and you strain a completely different set of tissues. Every single step sends a jolt of unnatural force and torque through an ankle joint that simply wasn't built to handle it. Over time, this constant misuse leads to its own inflammation, strain, and eventually, a persistent ache around the ankle.
Your limp isn't just a symptom of the heel pain—it's the direct cause of your next problem. By forcing your ankle to move in ways it shouldn't, you're overloading its support system and kicking off a new cycle of pain and inflammation.
The Domino Effect in Action
This isn't just a theory; it's a chain reaction we see all the time. Podiatrists regularly observe patients changing their gait to offload a painful heel, which then leads to abnormal stress on the ankle. As explained in resources like this one from RNV Podiatry, this compensation is a direct cause of secondary ankle pain.
These compensatory movements usually show up in a few common ways:
- Walking on the outer edge of your foot: This is a classic move that overworks the peroneal tendons, causing that dull, persistent ache on the outside of your ankle.
- Shifting your weight forward onto your toes: Doing this can strain your Achilles tendon and the ligaments at the front of the ankle.
- Taking shorter, more tentative steps: This choppy motion prevents your ankle from absorbing shock properly, which can irritate the joint itself.
The bottom line is that the ankle pain you're feeling is your body's cry for help, triggered by its attempt to protect your heel. To truly fix the ankle issue, you have to go back to the source and treat the plantar fasciitis first.
Is It Your Heel or Your Ankle? Understanding the Pain
When your lower leg starts aching, figuring out the exact source can be a real puzzle. Is it your heel? Your ankle? Or somehow both? Telling the difference between classic plantar fasciitis pain and the secondary ankle pain it can cause is your first step toward getting relief.

The hallmark of plantar fasciitis is a very specific, sharp pain right under your heel. Most people I've talked to describe it as a stabbing sensation, especially with those first few steps out of bed in the morning. It's an unmistakable, "get your attention" kind of pain.
On the other hand, the ankle pain that shows up because of plantar fasciitis feels different. It's usually a dull, nagging ache that settles in around the ankle. This discomfort tends to get worse as the day goes on because your funny walk—the one you adopted to avoid heel pain—is putting a slow, steady strain on your ankle joint.
Symptom Checker: Plantar Fasciitis vs. Related Ankle Pain
To help you sort things out, here’s a quick comparison of what you might be feeling.
| Symptom | Plantar Fasciitis (Heel) | Compensatory Ankle Pain |
|---|---|---|
| Location | Right under the heel, sometimes extending into the inner arch. | Around the ankle joint itself, often felt on the outer side. |
| Pain Type | Sharp, stabbing, or like a deep bruise. | A dull, persistent ache that feels tired and sore. |
| Worst Time | Those first steps after resting, especially in the morning. | Builds gradually with more time spent walking or standing. |
| Swelling | Usually minimal, maybe some slight puffiness under the heel. | More obvious swelling can appear around the whole ankle. |
This table is a good starting point, but keep in mind that other issues can feel similar. A simple ankle sprain or underlying arthritis can also cause discomfort. Sometimes, the pain might even be coming from your Achilles tendon. You can learn more about the signs of Achilles tendinopathy to see if that sounds more like your situation.
Crucial Takeaway: If your ankle is severely painful, looks very swollen, or just isn't getting any better, it's time to see a doctor. You need to rule out a separate injury and get a proper diagnosis. A clear conversation with a healthcare professional is the best way to get on the right treatment path.
Actionable Strategies for Relieving Both Pains
When you're dealing with pain in two places at once, finding a solution can feel overwhelming. But it’s simpler than you might think. The key to stopping that secondary ankle pain is to address the real problem: the plantar fasciitis in your heel.
Think of it as a domino effect. By focusing on healing the inflamed plantar fascia, you allow your natural walking pattern to return. Once your gait is back to normal, the unnatural strain on your ankle disappears, and that nagging ache finally gets a chance to fade away.
Your Action Plan for Heel and Ankle Relief
So, where do you start? The most effective approach combines immediate relief with long-term support to break the cycle of pain for good.
It's not just a hunch; it's a recognized strategy. A Dutch study on heel pain found that advising patients on insoles was a common treatment, used in 16.4% of cases, alongside other conservative methods. This shows that experts agree: correcting foot mechanics is a vital part of recovery. You can learn more about these common treatment approaches for heel pain.
Here’s a solid plan to get you started:
- Gentle Stretching: Regularly stretching your calves and the bottom of your feet is non-negotiable. Tight calf muscles pull on your heel, adding tension to the plantar fascia. Simple, gentle stretches can make a world of difference by improving flexibility and easing that strain.
- The RICE Method: When you have a painful flare-up in your heel or ankle, fall back on the classic RICE method: Rest, Ice, Compression, and Elevation. It’s a tried-and-true way to reduce inflammation and get some quick, temporary relief.
- Supportive Footwear: It's time to say goodbye to flimsy, flat shoes. Opt for footwear that has good arch support and a cushioned heel. This helps absorb the daily impact of walking and gives your feet the protection they desperately need.
The most powerful tool in your arsenal is often what's inside your shoes. Correcting your foot's mechanics is essential, and that’s where orthotic insoles come in.
Insoles work by giving you targeted arch support and heel cushioning right where you need it. This not only absorbs shock but also helps guide your foot back into a more natural alignment.
By fixing your mechanics from the ground up, insoles allow your gait to normalize, taking pressure off both your overstressed plantar fascia and your strained ankle. This is how you address the root cause, not just chase the symptoms. For more tips, check out our complete guide on what to do for plantar fasciitis.
Common Questions About Plantar Fasciitis and Ankle Pain

When you're dealing with foot and ankle pain, it’s natural to have a lot of questions. Let’s tackle some of the most common ones to give you a clearer picture of what's happening and how you can get back on track.
How Long Until My Ankle Pain Improves?
The short answer is: your ankle will start feeling better once your heel does. The ankle pain is a side effect, so as soon as you start treating the plantar fasciitis, your walking pattern can begin to return to normal.
Many people feel a noticeable difference in their ankle strain within a few weeks of consistent treatment, like daily stretching and wearing supportive insoles. If your heel pain improves but the ankle pain sticks around, it's a good idea to see a doctor. They can check if there's a separate issue with your ankle that needs attention.
Can My Shoes Make Both Conditions Worse?
Yes, absolutely. The wrong shoes are often a major culprit. Think about those flimsy, flat shoes with zero arch support—they do more harm than good, forcing your feet into unnatural positions and making both your plantar fasciitis and the related ankle pain worse.
Investing in structured shoes with a firm heel and solid arch support is one of the most powerful changes you can make. This single step helps both your heel and your ankle recover by providing the stability your feet desperately need.
What Kind of Doctor Should I See for This Pain?
For a first look, your primary care physician is a great place to start. They can give you an initial assessment and help you understand the basics.
However, to really get to the bottom of it, you'll want to see a specialist. A podiatrist, who is a foot and ankle expert, or an orthopedic specialist will give you the most accurate diagnosis. They can perform a gait analysis, recommend custom orthotics if necessary, and create a complete treatment plan to tackle the root problem for good.
Ready to break the pain cycle? Samurai Insoles were designed by a podiatrist to fix the faulty foot mechanics that cause plantar fasciitis, relieving both heel and ankle strain. Find the right support for your feet and start walking comfortably again.



